-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Cystectomy
Cystectomy
Cystectomy
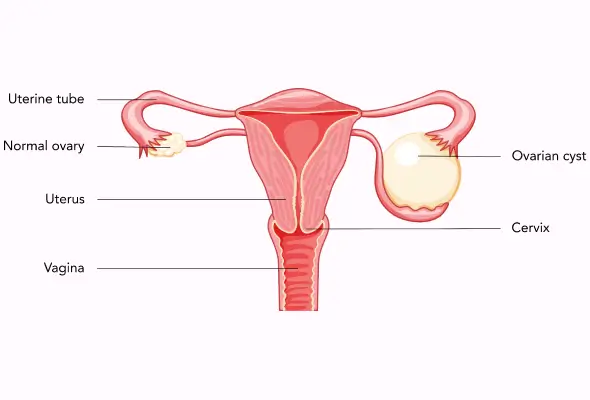
A cystectomy is a surgical procedure that removes the urine bladder. In men, removing the whole bladder (radical cystectomy) usually entails removing the prostate and seminal vesicles as well. In women, radical cystectomy includes the removal of the uterus, ovaries, and a portion of the vaginal wall.
Following the removal of your bladder, your surgeon will need to establish a urinary diversion – a new mechanism for urine to be stored and expelled from your body. Urine can be held and discharged in a variety of ways following bladder removal surgery. Your doctor can advise you on the best strategy for you.
Cystectomy Surgery is frequently used to treat aggressive or recurring noninvasive bladder cancer treatment. Other pelvic malignancies, such as advanced colon, prostate, or endometrial cancer, and some noncancerous (benign) disorders, such as interstitial cystitis or congenital anomalies, may also be treated with a cystectomy.
Diagnosis at CARE Hospitals
Your surgeon may suggest one of the following techniques for your surgery:
-
The procedure is open. To reach the pelvis and bladder, a single incision on your belly is required.
-
Minimally invasive surgery - To reach the abdominal cavity, your surgeon creates multiple small incisions on your belly through which specific surgical tools are placed.
-
You are given a medication (general anesthetic) that will keep you sleeping during the procedure. Once you're sleeping, your surgeon makes a big incision in your belly for open surgery or numerous smaller incisions for minimally invasive surgery.
-
Your bladder and adjacent lymph nodes are then removed by your surgeon. Other organs around the bladder, such as the urethra, prostate, and seminal vesicles in males, and the urethra, uterus, ovaries, and portion of the vagina in women, may also need to be removed by your surgeon.
Following the removal of your bladder, your surgeon will strive to repair the urinary system so that urine can exit your body. There are several alternatives available:
-
The ileal conduit. During this treatment, your surgeon will use a portion of your small intestine to form a tube that connects your kidneys to an opening in your abdominal wall by attaching it to the ureters (stoma). Urine pours out of the orifice in a steady stream. A bag that is worn on your belly clings to your skin and catches urine until it is emptied.
-
Reconstruction of the neobladder. Your surgeon will utilize a slightly bigger segment of your small intestine than the one used for an ileal conduit to build a sphere-shaped pouch that will become your replacement bladder during the development of a neobladder. The neobladder is implanted in the same area within your body as your original bladder, and it is connected to the ureters so that urine may flow from your kidneys. The opposite end of the neobladder is connected to your urethra, allowing you to urinate normally.
-
A neobladder is not a brand-new, normal bladder. If you have this surgery, you may need to use a catheter to assist drain the neobladder more effectively. In addition, some persons have urine incontinence following surgery.
-
Your surgeon will use a portion of your intestine to construct a tiny reservoir inside your abdominal wall during this treatment. The reservoir fills as you create pee, and you empty it multiple times each day with a catheter.
You eliminate the need to wear a urine collecting bag on the exterior of your body with this sort of urinary diversion. However, you will need to drain the internal reservoir multiple times each day using a long, thin tube (catheter). Leakage from the catheter site may create complications or need a return to the operating room for revision surgery.
Following the process
After the ovarian cystectomy surgery in Hyderabad, you may need to stay in the hospital for up to five or six days. This period is needed for your body to heal after the procedure. Because the intestines are usually the last portion of the body to wake up after surgery, you may need to stay in the hospital until your intestines are able to absorb fluids and nutrients again.
Side effects of general anesthesia include sore throat, shivering, tiredness, dry mouth, nausea, and vomiting. These may linger for a few days, but they should subside. Your healthcare provider may instruct you to get up and walk frequently beginning the morning following surgery. Walking promotes healing and the restoration of bowel function, increases circulation, and aids in the prevention of joint stiffness and blood clots.
For a few weeks following surgery, you may have pain or discomfort around your incision or incisions. Your pain should progressively improve as you recuperate. Before leaving the hospital, consult with your doctor about medications and other strategies to increase your comfort.
Our Doctors
-

Dr. Aditi Laad
MBBS, DNB
Woman & Child Institute
View More -

Dr. Chetna Ramani
MBBS, DGO
Woman & Child Institute
View More -
Dr. Sushmita Mukherjee Mukhopadhyay
MBBS, DGO, MD, DNB, FICOG
Woman & Child Institute
View More -

Dr. Neena Agrawal
MBBS, MS, FICOG, Diploma in Gynaecology, Endoscopy
Woman & Child Institute
View More -

Dr. Abhinaya Alluri
MS (OBG), FMAS, DMAS, CIMP
Woman & Child Institute
View More -

Dr. Alakta Das
MBBS, MS (O&G), FMIS
Woman & Child Institute
View More -
Dr. Alka Bhargava
MBBS, MS
Woman & Child Institute
View More -

Dr. Amatunnafe Naseha
MBBS, DNB, FRM
Woman & Child Institute
View More -

Dr. Aneel Kaur
DGO
Woman & Child Institute
View More -

Dr. Anjali Masand
MBBS, MD (OBG)
Woman & Child Institute
View More -

Dr. Arjumand Shafi
MBBS, DGO
Woman & Child Institute
View More -

Dr. Kranthi Shilpa
MBBS, MS (ObGyn), Fellowship in Infertility
Woman & Child Institute
View More -

Dr. Krishna P Syam
MBBS, DGO, DNB
Woman & Child Institute
View More -

Dr. M Sirisha Reddy
MBBS, MS OBGY
Woman & Child Institute
View More -

Dr. Maleeha Fatima
MBBS,DGO, DNB (Obstetrics and Gynaecology)
Woman & Child Institute
View More -
Dr. Maleeha Raoof
MBBS, DGO (Osmania University), DGO (University of Vienna), MRCOG
Woman & Child Institute
View More -

Dr. Manjula Anagani
MBBS, MD (Obstetrics & Gynecology), FICOG
Woman & Child Institute
View More -

Dr. Muthineni Rajini
MBBS, DGO, DNB, FICOG, ICOG, Certified Course in Gynecological Endoscopy
Woman & Child Institute
View More -

Dr. N Sarala Reddy
MBBS, MS (OBS & GYN), Diploma in IVF & Reproductive Medicine
Woman & Child Institute
View More -

Dr. Neha V Bhargava
MS, DNB (obgyn), MNAMS, Fellow (Gynae Oncology)
Woman & Child Institute
View More -
Dr. Prabha Agrawal
MBBS, MD, FMAS, FICOG, Fellowship in minimal access surgery
Woman & Child Institute
View More -

Dr. Prathusha Kolachana
MBBS, MS (Obstetrics and Gynecology), Post-Doctoral Fellowship in Endogynecology (Laparoscopy)
Woman & Child Institute
View More -

Dr. Ruchi Srivastava
MBBS, DGO, DNB
Woman & Child Institute
View More -
Dr. S V Lakshmi
MBBS, DGO, DNB (OBGYN)
Woman & Child Institute
View More -

Dr. Shabnam Raza Akther
MBBS, MD, DNB
Woman & Child Institute
View More -
Dr. Shreeja Gurrala
MBBS, M.S Obstetrics and Gynaecology, FMAS, DMAS, FRM, Fellow in ART, Post Doctoral Fellowship in Urogynaecology
Woman & Child Institute
View More -

Dr. Sirisha Sunkavalli
MBBS, DNB (OBG), FMAS, CIMP, Fellowship in Urogynecology
Woman & Child Institute
View More -

Dr. Sonal Lathi
MBBS, MD, DNB
Woman & Child Institute
View More -

Dr. Sushma J
MBBS, MS (OBG)
Woman & Child Institute
View More -

Dr. Swapna Mudragada
MBBS, DGO, MS
Woman & Child Institute
View More
Frequently Asked Questions
Still Have a Question?

