-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Congenital Anomaly of Uterus
Congenital Anomaly of Uterus
Congenital Uterus Treatment in Hyderabad, India
Congenital anomalies of the uterus are the congenital malformations in the uterus that develop during embryonic life. A uterine anomaly is when a woman’s uterus develops differently when in the womb. Less than 5% of women have congenital anomalies of the uterus, however, it has been observed that 25% of women who experienced miscarriage or preterm delivery have a congenital uterine anomaly.
Why does a congenital anomaly of the uterus occur?
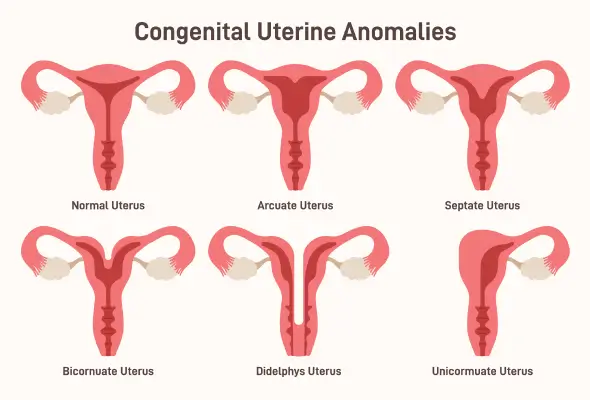
Types of congenital uterine anomalies
There are various types of congenital uterine anomalies, including –
-
Septate uterus – In this condition, the uterus appears normal from the surface, but it is divided into two different halves by a septum, on the inside. The septum can be of any size and thickness. Septate uterus is one of the most commonly diagnosed congenital uterine anomalies, responsible for 45% of all congenital uterine anomaly cases.
-
Arcuate uterus – In this condition, the uterus appears normal from the outside, but there is a shallow groove of 1 cm or less in the internal surface of the endometrial cavity. These kinds of anomalies make up for 7% of all congenital uterine anomalies.
-
Bicornuate uterus – In this condition, the uterus has a groove on the external surface and has two endometrial cavities. The uterus appears to be separated into two halves, excluding the lower part. The bicornuate uterus makes up for 25% of all congenital uterine anomalies.
-
Unicornuate uterus – In this condition, only half of the uterus has developed from one Mullerian duct, making up for 15% of all congenital uterine anomalies.
-
Uterine agenesis – In this condition, the uterus fails to develop. This condition is prevalent in 10% of all women with congenital uterine anomalies.
-
Uterus didelphys – In this condition, the two halves of the uterus develop completely separate, making up for 7.5% of all congenital uterine anomaly cases.
The most common congenital uterine anomalies are septate and bicornuate uterine anomalies.
Symptoms
Typically, there are no symptoms of congenital uterine anomalies. Most women don’t discover that they have a congenital uterine anomaly until they get their first prenatal ultrasound or diagnosis of infertility. In case when symptoms do appear, these include:
- Painful periods – Due to congenital anomalies of the uterus, there may be an obstruction in menstrual bleeding. This leads to abdominal pain and cramps.
- Complete absence of periods – Due to uterine anomalies, severe intrauterine scarring can occur, due to which adhesions can form on the walls of the uterus. This leads to the uterine walls sticking to each other and the endometrial lining becoming very thin. This in turn prevents the embryo from attaching itself to the uterus. In severe cases, menstrual bleeding may stop completely.
- Recurrent miscarriages – Due to congenital uterine anomalies such as a septate uterus, it becomes difficult for women to sustain their pregnancies, leading to recurrent miscarriages.
- Breech or transverse baby position – Sometimes, due to congenital uterine anomalies, the baby’s position becomes transverse or breech wherein, instead of its head, the baby’s feet face downward. In such cases, a C-section is recommended.
- Pain during intercourse – Congenital uterine anomalies can lead to painful intercourse. It can also make it uncomfortable to insert a tampon.
- Preterm labour – Uterine anomalies can cause preterm labour, increasing the risk of infection for newborns and can also cause developmental problems in them.
Causes
In most cases of congenital uterine anomalies, the cause is unknown. More than 90% of women with uterine anomalies have a normal number of chromosomes. However, between 1938 and 1971, to prevent miscarriages and premature deliveries, some pregnant women were treated with DES (diethylstilbestrol). It was observed that these women were at an increased risk of having a congenital uterine anomaly. Other than this, there haven’t been any well-established risk factors, as of now.
-
Septate uterus – The exact cause behind a septate uterus isn’t known. It occurs while the embryo is developing. When the two tubes that are supposed to fuse to form the uterus don’t fuse effectively, a septate uterus occurs.
-
Bicornuate uterus – Also known as a heart-shaped uterus, a bicornuate uterus is when the uterus appears to be heart-shaped. A woman is born with this condition. The special ducts fuse only partially. This leads to the separation of the two upper parts of the uterus, also known as horns. These horns stick out a little, giving the uterus a heart-shaped appearance.
-
Unicornuate uterus – A unicornuate uterus is when only one-half of the uterus forms. It is also known as a single-horned uterus and has only one fallopian tube. It occurs when the uterus doesn’t develop properly during fetal development. When one of the two Mullerian ducts fails to develop, a unicornuate uterus is formed. Healthcare providers haven’t been able to identify why some women have a unicornuate uterus.
-
Uterine agenesis – When a baby’s reproductive system fails to develop while she’s in the womb, the condition is called uterine agenesis. It is generally a symptom of a broader condition that involves several abnormalities of the reproductive system, such as MRKH syndrome, MURCS association, or AIS. The cause of this congenital uterine anomaly isn’t known yet.
-
Uterus didelphys – In this condition, the two Mullerian ducts go on to become two separate uteruses. It is a rare congenital uterine anomaly and its cause isn’t known. Genetic components may be a factor as in some cases, this condition runs in families.
About 6.7% of the general population have congenital uterine malformations. However, its prevalence is higher in women with infertility problems and even higher in women who have a history of recurrent miscarriages. Due to uterine anomalies, there is a negative effect on a woman's ability to carry out their pregnancy to full term. About 1 in 4 women who have had miscarriages or preterm births have uterine malformations.
Consequences of Abnormal Uterus
Uterine abnormalities or malformations, such as Congenital anomaly of the uterus can have various consequences and may impact reproductive health and overall well-being. The specific consequences can vary depending on the type and severity of the anomaly. Here are some potential consequences:
- Fertility Issues: Certain uterine anomalies can affect fertility. For example, a septate uterus (a uterus divided by a septum) may increase the risk of recurrent pregnancy loss or difficulty conceiving.
- Increased Risk of Pregnancy Complications: Uterine anomalies can be associated with a higher risk of pregnancy complications, such as preterm birth, breech birth, or cesarean section. The risk depends on the type of anomaly and its impact on the uterine structure.
- Miscarriage: Women with certain uterine anomalies, such as septate or bicornuate uterus, may have a higher risk of miscarriage. The altered uterine structure can impact implantation and the development of the fetus.
- Menstrual Irregularities: Some uterine anomalies, such as a double uterus or septate uterus, may lead to menstrual irregularities, including heavy or painful periods. These anomalies can affect the normal shedding of the uterine lining.
- Obstructed Labor: In some cases, certain uterine anomalies may lead to obstructed labor during childbirth. This can increase the risk of complications for both the mother and the baby.
- Increased Risk of Gynecological Issues: Women with uterine anomalies may be at a higher risk of certain gynecological issues, such as endometriosis or reproductive tract infections.
- Psychological Impact: Dealing with fertility challenges, pregnancy complications, or recurrent miscarriages due to uterine anomalies can have a significant psychological impact on individuals and couples. Seeking emotional support and counseling may be important in such situations.
Diagnosis
Congenital uterine anomalies can be recognized at the onset of a girl’s puberty, when menstruation begins, or when it fails to begin. Congenital anomalies of the uterus can also be diagnosed when a woman has infertility problems or trouble sustaining her pregnancy. For an accurate diagnosis and Bicornuate / Septate Uterus Treatment in Hyderabad, a combination of tests may be performed. These tests include complete medical history, physical examination, and imaging tests such as a 3D ultrasound, hysterosalpingogram, and MRI.
-
Septate uterus – A septate uterus can be diagnosed with a standard 2D pelvic ultrasound. An MRI might be a more accurate test to diagnose further issues of the uterus. To confirm a septate uterus, a hysteroscopy or a hysterosalpingogram is performed. In a hysterosalpingogram, the inner uterus and fallopian tubes are highlighted. In a hysteroscopy, a thin instrument with light is inserted into the vagina, all the way through the cervix to obtain a clear view of the uterus. After diagnosis, one must see a consultant to get help regarding septate uterus treatment.
-
Bicornuate uterus – A bicornuate uterus can be diagnosed with a pelvic exam, an ultrasound, an MRI, and a hysterosalpingogram. It is most commonly detected during a prenatal ultrasound or an ultrasound for other unwanted symptoms. Many women go about their whole lives without discovering that they have a bicornuate uterus. After the diagnosis is done, they have to see a professional to get bicornuate uterus treatment.
-
Unicornuate uterus – Many times, a unicornuate uterus goes undetected until a woman has trouble getting pregnant or experiences complications during pregnancy. A unicornuate uterus can be diagnosed with a regular physical exam, thorough medical history, and a pelvic exam. Apart from this, imaging tests such as an ultrasound, an MRI or laparoscopy, and hysteroscopy may also be performed.
-
Uterine agenesis – Usually, this condition isn’t diagnosed until puberty when a girl fails to have periods. Until then, it isn’t diagnosed since the outward genitals appear normal. Uterine agenesis can be diagnosed with a pelvic exam, thorough medical history, blood tests, ultrasound, and MRI. After that, they must seek uterine agenesis treatment.
-
Uterus didelphys – Uterine didelphys or double uterus can be diagnosed with a routine pelvic exam, when your doctor suspects or observes an abnormally shaped uterus or a double cervix. The diagnosis can be further confirmed with an ultrasound, MRI, hysterosalpingography, or a sonohysterogram. One mustseek professional help regarding the uterus didelphys treatment after the diagnosis.
Treatment
Congenital uterine anomalies can only be treated with surgery. However, some women don’t require any treatment if the anomaly doesn’t interfere with their pregnancy. In most cases, women with a congenital anomaly of the uterus don’t experience any reproductive or medical problems. For those that require surgery, the type of surgery that is done depends on the type of congenital anomaly of the uterus.
-
Septate uterus – A septate uterus can be treated with metroplasty. In this surgery, a lighted instrument is inserted into the uterus, through the vagina and cervix. Another instrument is inserted to cut away and remove the septum. It is a minimally invasive procedure that takes about an hour. Most women can return home on the same day as their metroplasty surgery. After this surgery, 50% to 80% of women with a history of recurrent miscarriages can achieve healthy pregnancies in the future. Hence, the chances of successful pregnancy increase with this surgery.
-
Bicornuate uterus – To correct a bicornuate uterus in women with a history of recurrent miscarriages, Strassman metroplasty surgery is performed. However, surgery isn’t required in a majority of women with a bicornuate uterus. According to a study, 88% of women who underwent Strassman metroplasty were able to achieve successful pregnancies. A bicornuate uterus doesn’t affect a woman’s fertility, however, it might cause problems such as early miscarriage or early birth. Although, it is still possible to achieve successful pregnancy and delivery.
-
Unicornuate uterus – In some cases, women with a unicornuate uterus also have a smaller hemi-uterus. Doctors recommend that a hemi-uterus should be surgically removed as a pregnancy might begin there. Such a pregnancy isn’t viable since the area is much smaller and the hemi-uterus could rupture, making it a potentially life-threatening situation. To reduce the risk of miscarriage, cervical cerclage is also recommended, if a woman has cervical shortening. Certain medications might also be prescribed to reduce the likelihood of preterm delivery.
-
Uterine agenesis – Depending on the individual and their symptoms, there are various treatment options available for uterine agenesis. If the vagina is also missing along with the uterus, a vagina can be reconstructed through vaginal dilators or reconstructive surgery.
-
Uterus didelphys – In the case of the double uterus, treatment is rarely needed if there aren’t any symptoms or signs. If there is a partial division within the uterus, surgery to unite a double uterus can be performed to sustain a pregnancy. If you have a double vagina along with a double uterus, surgery to remove the wall of tissue that separates the two vaginas can also be performed to make childbirth easier.
In the case of a unicornuate, bicornate, or didelphic uterus, usually, surgery isn’t recommended. Surgery to treat the septate uterus is only recommended if a woman faces reproductive issues. It can be corrected by removing the septum surgically. This improves the chances of a positive pregnancy outcome. Surgery to treat a congenital uterine anomaly can repair the defect, and thereby eliminate discomfort during periods or sexual intercourse. It can also improve fertility as well as pregnancy outcomes. If a woman with a congenital anomaly of the uterus is having trouble achieving pregnancy within six months of trying, she should see a fertility specialist.
Still Have a Question?

