-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Uterine Fibroids
Symptom, Causes, Diagnosis and Treatment
Uterine Fibroids
Uterine fibroids are common growths in the women's uterus. They are mostly asymptomatic. But sometimes, they can cause a few health issues. Let us unfold each chapter about uterine fibroids in an easy-to-understand manner.
What are Uterine Fibroids?
Uterine fibroids are non-cancerous growths. They can vary in size, from tiny fibroids in the uterus to large masses. They have uterine muscle cells and fibrous connective tissue and can occur either as a single mass or in clusters.
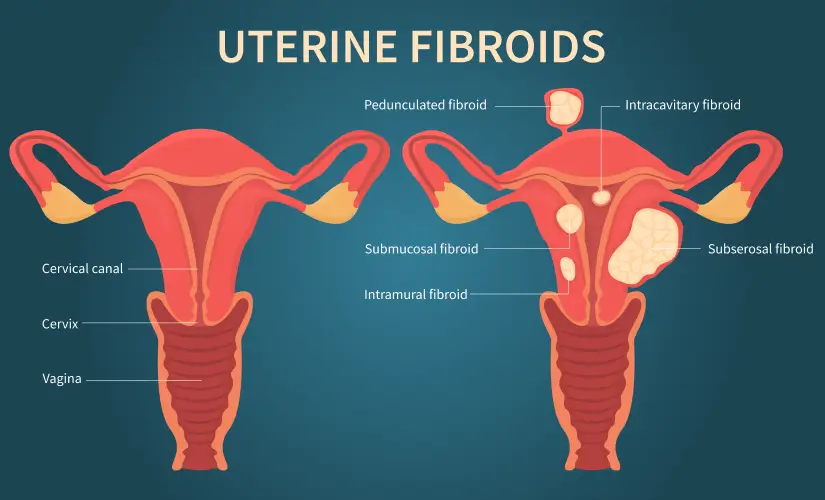
Types of Uterine Fibroids
There are several types of uterine fibroids, based on their location within the uterus, including:
- Intramural fibroids: They are the most common type of uterine fibroids that can grow inside the uterine muscular wall.
- Subserosal uterine fibroids: These fibroids develop on the uterine outer surface and can sometimes grow on a stalk (becoming pedunculated).
- Submucosal fibroids: They are called submucosal fibroids since they grow beneath the endometrium (the inner lining of the uterus). They can protrude into the uterine cavity.
- Pedunculated fibroids: These fibroids grow on a stalk-like structure inside or outside the uterus.
Symptoms of Uterine Fibroids
The symptoms of uterine fibroids can vary depending on the size of the fibroid, location, and number of fibroids present. Some women may experience no symptoms at all, while others may suffer from heavy or prolonged menstrual bleeding, pelvic pain or pressure, irregular urination or difficulty emptying the bladder, bloating or constipation, backache or leg pain, and reproductive issues, such as infertility or miscarriage.
What is the cause of the development of uterine fibroids?
The exact reason for fibroids in the uterus remains unknown most of the time, but several factors may contribute to their development, such as:
- Hormones: According to some research, estrogen and progesterone, the two primary female hormones, play a crucial role in the growth of uterine fibroids. When the levels of these hormones decrease after menopause, fibroids tend to shrink.
- Genetics: Women with a family history of uterine fibroids are more likely to develop them.
- Race: African American women are more prone to developing uterine fibroids than women of other racial groups.
- Age: Fibroids typically develop during the reproductive years, with the risk increasing as women approach menopause.
- Other factors, such as early menstrual onset, obesity, hypothyroidism, and certain dietary habits, may also contribute to the development of uterine fibroids.
Diagnosis
Some women with uterine fibroids may experience no symptoms at all, and the doctor may discover the condition during a routine pelvic examination or imaging test. Some of the diagnostic tests are:
- Pelvic evaluation: During a pelvic exam, your doctor may feel the presence of fibroids in the uterus.
- Ultrasound: Transvaginal or abdominal ultrasound can provide overall images of the uterus and any fibroids present.
- Magnetic Resonance Imaging (MRI): An MRI can provide highly detailed images of the uterus and fibroids, helping to determine their size, location, and number.
- Hysteroscopy: This medical procedure involves inserting a thin, lighted catheter through the cervix to examine the inside of the uterus.
Uterine Fibroid Treatments
Several factors can influence the treatment plan for uterine fibroids, including but not limited to the severity of symptoms, the size and position of the fibroids, and the woman's age and desire for future pregnancy. Treatment options include:
- Watchful waiting: If the uterine fibroids are small and asymptomatic, your doctor may suggest regular monitoring without immediate treatment.
- Medication: Certain medicines, such as gonadotropin-releasing hormone (GnRH) agonists or non-steroidal anti-inflammatory drugs (NSAIDs), can help manage symptoms like heavy bleeding or pelvic pain.
- Minimally invasive procedures:
- Uterine artery embolization (UAE): This procedure obstructs the blood supply to the fibroids, leading them to shrink.
- Magnetic Resonance-guided Focused Ultrasound Surgery (MRgFUS): MRgFUS is a noninvasive procedure that uses high-intensity focused ultrasound waves to destroy fibroid tissue.
- Endometrial ablation: It destroys the uterus lining, reducing heavy bleeding associated with fibroids.
- Surgery:
- Myomectomy: This surgical procedure removes the fibroids while
- preserving the uterus, making it an option for women who wish to become pregnant in the future.
- Hysterectomy: Surgeons typically recommend this surgical removal of the uterus for women with severe symptoms or huge fibroids who do not want to preserve their fertility.
Complications of Uterine Fibroids
While uterine fibroids are generally benign, they can sometimes lead to complications, such as heavy or excessive menstrual bleeding, pelvic pain or pressure due to an enlarged fibroid uterus, reproductive issues, and urinary or bowel problems. Fibroids may put pressure on the urinary bladder or rectum, resulting in frequent urination, difficulty emptying the bladder, constipation, or, in severe cases, bowel obstruction and severe pain or fever.
When to see a doctor
If you experience any of the following symptoms, it's essential to consult with your doctor:
- Heavy or prolonged menstrual bleeding
- Pelvic pain or pressure
- Frequent urination or difficulty emptying the bladder
- Constipation or bloating
- Reproductive problems, such as recurrent miscarriage or infertility
Prevention
While there is no guaranteed way to prevent uterine fibroids, certain lifestyle changes may help reduce your risk, including:
- Maintain a healthy weight: Being overweight or obese increases the risk of developing fibroids. Therefore, try to maintain a healthy weight through diet and exercise. Regular physical activity, such as walking, power yoga, cycling, and swimming, can maintain a healthy weight and may reduce the risk of fibroids.
- Eat a balanced meal: A diet rich in organic fruits, fresh vegetables, and whole grains may help reduce the risk of fibroids.
- Limit alcohol intake: Excessive alcohol consumption has been linked to an increased risk of fibroids.
- Manage stress: Chronic stress may contribute to developing fibroids, so finding healthy ways to manage stress is essential. You can incorporate yoga, meditation, deep breathing exercises, or walking in nature into your daily routine.
- Regular check-up: Routine gynecological check-ups may help detect fibroids early. Early detection and medical treatment may prevent complications associated with large or symptomatic fibroids.
Conclusion
Uterine fibroids are a common condition affecting women before the age of 50. They are non-cancerous and, in some cases, can cause manifestations like heavy menstrual bleeding, pelvic pain, and other reproductive issues. While the exact cause is unknown, but hormones, genetics, and age play a
key role in their development.
FAQS
1. Which size of fibroid is dangerous?
Fibroids rarely become dangerous. However, larger fibroids (those larger than 3-4 inches in diameter) can cause severe symptoms and complications.
2. What is the leading cause of fibroids?
The exact fibroid uterus reason is unknown, but numerous factors lead to their development, including hormonal fluctuations (estrogen and progesterone), genetics, race, age, obesity, and early onset of menstruation. It is also associated with Hypothyroidism.
3. What happens if fibroids go untreated?
If left untreated, uterine fibroids can continue to grow and cause various complications, such as heavy menstrual bleeding, pelvic pain or pressure, reproductive issues, urinary or bowel problems, and, in rare cases, degeneration of the fibroids, leading to severe pain or fever.
4. Can fibroids change over time?
Yes, uterine fibroids can change over time. Fibroids may grow larger or shrink depending on various factors, including hormonal changes, age, and the individual's overall health.
To Book an Appointment, call:
Still Have a Question?




