-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Ulcerative Colitis
Symptom, Causes, Diagnosis and Treatment
Ulcerative Colitis
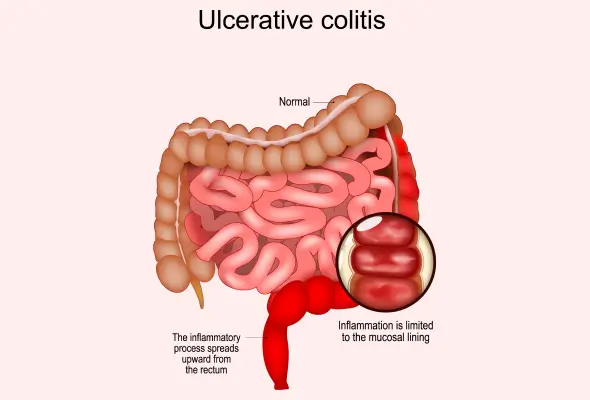
Ulcerative colitis is a chronic medical condition that has an impact on the lives of millions worldwide. This inflammatory bowel disease causes inflammation & ulcers in the lining of the large intestine and rectum, resulting in a range of uncomfortable symptoms. Understanding ulcerative colitis is crucial to managing its effects and improving the quality of life for those affected.
Let's explore what ulcerative colitis is, its various types, and the common symptoms to watch out for. We'll also delve into the causes and risk factors, potential complications, and methods to diagnose ulcerative colitis.
What is Ulcerative Colitis?
Ulcerative colitis (UC) is a long-term inflammatory bowel disease (IBD) that affects the large intestine, specifically the colon and rectum. This long-term condition causes the immune system to attack the gut lining, resulting in inflammation and ulcers on the colon's inner surface.
The condition is characterised by periods of active symptoms, known as flare-ups or relapses, followed by periods of remission when symptoms subside. Ulcerative colitis can develop at any age, but it is most commonly diagnosed in people between 15 and 30 years old.
Types of Ulcerative Colitis
Ulcerative colitis (UC) can affect any parts of the colon and rectum, leading to various types of the condition. The three main types of UC are:
- Ulcerative Proctitis: Being the mildest form, ulcerative proctitis affects about one-third of people with UC. In this type, inflammation is limited to the rectum, typically involving less than 6 inches of the area.
- Left-sided Colitis: This type of UC causes inflammation from the rectum up to the splenic flexure, a bend near the spleen. This type includes proctosigmoiditis, where inflammation affects the rectum and sigmoid colon (the lower, S-shaped part of the colon).
- Extensive Colitis: Also known as pancolitis, extensive colitis is the most severe form. It affects the entire colon, with inflammation starting at the rectum and extending beyond the splenic flexure.
The severity of UC can vary from mild to moderate or severe, depending on the symptoms and extent of inflammation. In rare cases, a life-threatening form called fulminant ulcerative colitis may occur, requiring urgent medical attention.
Symptoms of Ulcerative Colitis
Ulcerative colitis symptoms can vary in severity and often worsen over time. These include:
- Recurring diarrhoea that may contain mucus, blood, or pus
- Abdominal pain
- Extreme fatigue
- Loss of appetite
- Weight loss
- Abdominal cramping
- Nausea
- Fever
In addition to intestinal symptoms, about 25% of people with ulcerative colitis develop extra-intestinal symptoms. These can include:
- Painful and swollen joints (arthritis)
- Mouth ulcers
- Irritated, red-eyes
- Skin-related issues such as painful bumps, rashes, or ulcers
The impact of ulcerative colitis on daily life can be significant for some people. Symptoms like urgent bowel movements and tenesmus (feeling the need to use the toilet but being unable to) can be particularly disruptive.
Causes and Risk Factors of Ulcerative Colitis
While the exact triggers for flare-ups are often unidentified, researchers believe it's a complex interplay of various factors. The most widely accepted theory suggests that ulcerative colitis (UC) is an autoimmune condition where the immune system mistakenly attacks healthy colon tissue, causing inflammation and damage.
Several risk factors have been identified that may increase the likelihood of developing ulcerative colitis. These include:
- Age plays a role, with most diagnoses occurring between 15 and 30 years old or after 60.
- Race and ethnicity also influence risk, with white individuals, particularly those of Ashkenazi Jewish descent, being more susceptible.
- Genetics has a significant impact on ulcerative colitis risk. Having a first-degree relative (mother or father) with the condition increases the chances of developing it.
- Environmental factors also contribute to the development of ulcerative colitis. A high-fat diet, stress, and smoking may worsen its symptoms.
- Other factors, such as urban living, certain medications, and a history of gastroenteritis, have been linked to an increased risk of ulcerative colitis.
Complications
Ulcerative colitis can lead to several serious complications that have an impact on a person's overall health and quality of life. These may include:
- Increased risk of developing bowel cancer, especially for those with severe or extensive colitis.
- Poor growth and development in children and young people
- Primary sclerosing cholangitis
- Toxic megacolon
- The use of steroid medicines to treat ulcerative colitis can cause osteoporosis as a side effect.
Diagnosis
To diagnose ulcerative colitis, doctors use a combination of methods, such as:
- Medical History: Doctors ask about your symptoms, factors that trigger UC flare-ups, and any additional symptoms.
- Physical Assessment: During this exam, the doctor may check vital signs, listen to abdominal sounds, and perform a digital rectal exam to check for blood in the stool.
- Blood Tests: They help identify signs of ulcerative colitis and potential complications like anaemia. These tests can also reveal signs of infection or other digestive diseases that may cause similar symptoms.
- Stool Tests: Patient stool is analysed for signs of inflammation in the intestines.
- Endoscopy: This diagnostic test allows doctors to view the lining of the large intestine and take tissue samples (biopsies) for further analysis.
Treatment for Ulcerative Colitis
The treatment for ulcerative colitis aims to reduce symptoms and maintain remission.
- Medications:
- Anti-inflammatory drugs, such as aminosalicylates (5-ASAs), are often the first line of treatment for mild to moderate ulcerative colitis. These medicines help reduce inflammation and can be administered orally, as suppositories, or through enemas.
- Corticosteroids are effective in reducing inflammation, but they are not suitable for long-term use due to potential side effects.
- Immunosuppressants help treat flare-ups and maintain remission by reducing immune system activity.
- Biologic medicines target specific proteins in the immune system to reduce inflammation.
- Surgery: In cases where medications are ineffective or complications arise, doctors may suggest surgery. This involves removing the colon and rectum (proctocolectomy) and creating either an ileostomy or an internal pouch (ileoanal pouch) for waste elimination.
When to See a Doctor
- If you have symptoms of ulcerative colitis disease and haven't been diagnosed, it's crucial to see a doctor as soon as possible.
- For those already diagnosed with ulcerative colitis, immediately contact your doctor if you think you're having a severe flare-up.
- Seek medical help right away if you experience heavy, persistent diarrhoea, blood leaking from your anus with clots in your stool, constant pain, or a high fever.
- It's also important to contact your doctor if you notice any signs of infection, such as coughs, fever, or a sore throat.
Prevention
While it's not possible to prevent ulcerative colitis entirely, there are steps you can take to reduce the likelihood of flare-ups and manage the condition effectively. These include:
- Taking your medications exactly as prescribed is crucial. This is one of the best ways to keep ulcerative colitis under control and prevent flares.
- Certain medications can make ulcerative colitis symptoms worse. These include certain antibiotics and NSAIDs, which can cause inflammation in the intestines.
- Regular check-ups with your doctor are crucial, typically every six months while in remission. If you're having a flare-up, check in with your doctor promptly. They may need to run tests to rule out other potential causes of digestive symptoms, such as infections.
- Managing stress is another key aspect of preventing flare-ups. While stress may not directly cause flares, it can worsen digestive symptoms.
- Try to get at least seven hours of sleep a night, exercise regularly, and find healthy ways to relieve stress, such as meditation.
Conclusion
Ulcerative colitis is a challenging condition that has a significant impact on the lives of those affected. Remember, while there's no cure, various effective ulcerative colitis treatments can help control symptoms, reduce the frequency of flare-ups, and enhance the quality of life. Living with ulcerative colitis requires ongoing care and attention. Regular check-ups, proper medication management, and lifestyle adjustments are key to maintaining remission and preventing complications. Don't hesitate to contact your doctor if you experience symptoms or have concerns. With proper management and support, many people with ulcerative colitis can lead fulfilling lives and effectively cope with the challenges of this condition.
FAQs
1. How serious is ulcerative colitis?
Ulcerative colitis (UC) is a chronic gastrointestinal condition that can significantly affect a person's quality of life. While its severity varies, it can lead to serious complications like an increased risk of bowel cancer and poor growth in children. In rare cases, a severe form called fulminant ulcerative colitis can be life-threatening, requiring urgent medical attention.
2. Can ulcerative colitis go away?
Ulcerative colitis is a long-term condition that doesn't typically go away on its own. However, with proper treatment, many people experience periods of remission where symptoms subside. About 70% of patients respond well to medication and achieve remission. For those who don't respond to medication, surgery to remove the colon can effectively cure ulcerative colitis.
3. What is the leading cause of ulcerative colitis?
The exact cause of UC remains unknown. However, it's considered an autoimmune condition where the immune system mistakenly attacks healthy colon tissue. Researchers believe a combination of genetic and environmental factors likely triggers this abnormal immune response.
5. Why does colitis start?
While the precise trigger for ulcerative colitis is unclear, several factors may contribute to its onset. These include genetic predisposition, age (most diagnoses occur between 15-30 years), and ethnicity (it's more common in white people of European descent). Environmental factors and changes in the gut microbiome may also play a role in the development of the condition.
6. How long does colitis last?
Ulcerative colitis typically involves periods of flare-ups followed by remission. The duration of these periods can vary significantly from person to person. With proper treatment, many individuals can achieve long periods of remission. However, for some, symptoms may worsen over time, potentially leading to the need for surgery in up to 30% of cases.
Dr. Jagadeeswar S

Still Have a Question?



