-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Shingles
Symptom, Causes, Diagnosis and Treatment
Shingles
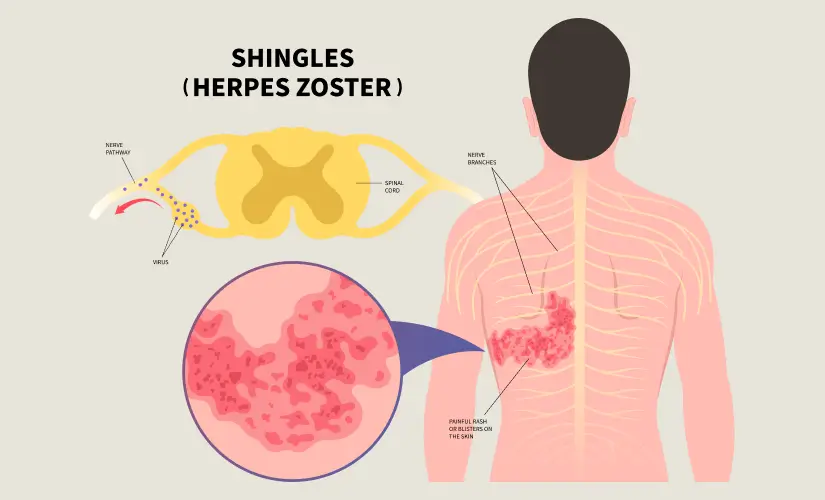
Shingles, medically known as herpes zoster, is a viral infection. This causative agent, varicella-zoster virus, can cause a painful, blistering rash. While it may seem like a straightforward condition, shingles can have a profound emotional and physical impact on those affected. This comprehensive blog aims to provide a deep understanding of shingles, its symptoms, shingles reasons, risk factors, and the various effective treatments available to manage this condition.
What are Shingles?
Shingles are caused by the varicella-zoster virus (VZV). This is the same virus that is responsible for chickenpox. If a person has a history of chickenpox, the varicella-zoster virus may remain in the nerve tissues of the infected person in the dormant stage for years. Shingles occur when the virus reactivates, often due to weakened immunity, stress, or ageing.
The primary characteristic of shingles is a painful, blistering rash. This rash is commonly present on one side of the body or face, following the path of the affected nerve. Before the blisters appear, the rash can be accompanied by tingling, itching, or burning sensations.
Symptoms of Shingles
The symptoms of shingles can vary in severity from person to person, but some common signs and symptoms include:
- Pain, burning or tingling sensation in a particular part of the body are among the early shingles symptoms
- Rash or blisters that appear in a band-like or stripe pattern on one side of the body
- Fever, chills, and headache
- Fatigue is one of the early shingles symptoms
- Itching or sensitivity to touch in the affected area
- Muscle weakness or paralysis (in rare cases)
It's essential to note that the pain associated with shingles can be intense and may persist even after the rash has healed (postherpetic neuralgia (PHN)).
What Causes Shingles?
The activation of the previously dormant varicella-zoster virus (VZV) is the leading cause of shingles. After recovering from chickenpox, the virus can lie dormant in the nerve cells for years or even decades. However, in some individuals, the virus can again become active due to various factors, such as:
- Age: The possibility of developing shingles increases as people get older, particularly after age 50.
- Weakened immune system: Various ailments that weaken the immune system, such as HIV/AIDS, cancer, or certain medications (e.g., chemotherapy, steroids), can increase the likelihood of shingles.
- Stress: High levels of stress can repress the immune system, making people more susceptible to viral reactivation.
- Certain medical conditions: Diseases like autoimmune disorders, diabetes, and cancer can increase the chance of shingles.
- Injury or trauma: Damage to the nerves or nerve roots can trigger the reactivation of the virus.
When to See a Doctor?
A doctor consultation is essential if you suspect you have shingles. Timely diagnosis and management can reduce the severity of symptoms and the likelihood of complications. Contact your doctor immediately if you experience the following:
- A rash or blisters accompanied by pain, tingling, or burning sensations Fever, chills, or general feeling of unwellness
- Rash or blisters near the eyes, as this can lead to complications and vision problems
- Severe pain that can cause poor sleep or interfere with daily activities
Complications
While shingles is generally a self-limiting condition, it can sometimes lead to several serious complications. These complications include:
- Postherpetic neuralgia (PHN): This is the most prevalent complication of shingles. PHN is characterised as persistent, severe pain in the affected area. A person may feel this pain even after the rash has healed.
- Vision problems: If the rash develops near the eyes, it can lead to complications such as corneal inflammation, vision loss, or even blindness.
- Bacterial skin infections: The blisters associated with shingles can become infected, leading to cellulitis or other skin infections.
- Neurological complications: In rare cases, shingles can cause several neurological complications, such as paralysis, encephalitis (brain inflammation), or meningitis (inflammation of the membranes surrounding the brain and spinal cord).
Prevention of Shingles
While there is no guaranteed way for shingles prevention, there are several measures that can help reduce the risk, including:
- Vaccination: The shingles vaccine, also known as Shingrix, is recommended for adults above 50. This vaccine can prevent shingles and reduce the chance of its complications.
- Boosting the immune system: Maintaining an active lifestyle, practising stress management, and getting plenty of rest can strengthen your immune system and reduce the risk of viral reactivation.
- Antiviral medications: Doctors may prescribe antiviral medicines to help prevent the development of shingles for individuals with weakened immune systems.
Diagnosis
Diagnosing shingles involves a physical examination and a review of the patient's medical history. The doctor will inspect the characteristic rash and assess the distribution of the blisters, which often follow the path of a specific nerve. Sometimes, doctors may conduct additional tests, such as a polymerase chain reaction (PCR) test or a viral culture, to confirm the diagnosis.
Treatment
The treatment for shingles aims to alleviate symptoms, prevent complications, and promote healing. Shingles treatment duration may vary depending on the severity of the infection. The following are some general treatment modalities:
Antiviral medications: Antiviral drugs can reduce the severity and duration of shingles symptoms, particularly if started within the first 72 hours of the rash appearing.
Pain management: Over-the-counter or prescription pain medicines may help manage the pain associated with shingles.
- Topical treatments: Calamine lotion, cool compresses, or numbing creams can help alleviate itching and discomfort caused by the rash.
- Corticosteroids: Doctors may sometimes prescribe corticosteroids to reduce inflammation and pain, mainly if the rash involves the eyes or other sensitive areas.
- Anticonvulsants or antidepressants: Doctors can also prescribe these medications to manage postherpetic neuralgia (PHN), a complication characterised by persistent, severe pain after the rash has healed.
Conclusion
Shingles is a painful and potentially debilitating ailment that significantly impacts an individual's physical and emotional well-being. Understanding the causes, symptoms, risk factors, and available treatments is crucial for effectively managing and preventing complications. By seeking prompt medical attention, following recommended shingles treatments, and taking preventive measures, individuals can reduce the severity of shingles and improve their overall quality of life. If you suspect you might have shingles or have any concerns about your risk, we encourage you to consult a healthcare professional.
FAQ's
1. What is the leading cause of shingles?
The main reason for shingles is the reactivation of the varicella-zoster virus (VZV), which remains in the inactive state in nerve cells of an individual with a history of chickenpox. In some individuals, the virus can become active later in life due to various factors, including ageing, a weakened immune system, stress, and certain medical conditions.
2. How long will shingles last?
The duration of shingles can vary, but most cases resolve within 3 to 5 weeks. However, some individuals may experience lingering pain or complications, such as postherpetic neuralgia (PHN), which can persist for months or even years after the shingles rashes have healed.
3. Why are shingles so painful?
Shingles are often accompanied by severe burning or tingling pain due to the virus affecting the nerves. The pain can be excruciating because the virus causes
inflammation and nerve damage, leading to the transmission of intense pain signals to the brain.
4. How common is shingles?
Shingles is a relatively common condition, affecting approximately one in three people in their lifetime. The shingles infection is more common in elderly people, with the highest prevalence in people over 50.
5. Who is at risk of getting shingles?
While anyone who has had chickenpox history can develop shingles infection, certain factors can increase an individual's risk, including:
- The risk of shingles increases significantly after the age of 50.
- Conditions or treatments that weaken the immune system, such as HIV/AIDS, cancer, chemotherapy, or long-term steroid use, can increase the risk of shingles. Chronic stress can significantly impact immunity, making individuals more susceptible to viral reactivation.
- Certain medical conditions like diabetes, autoimmune disorders, and cancer can lead to increased susceptibility to shingles.

Still Have a Question?



