-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Ocular Hypertension
Symptom, Causes, Diagnosis and Treatment
Ocular Hypertension
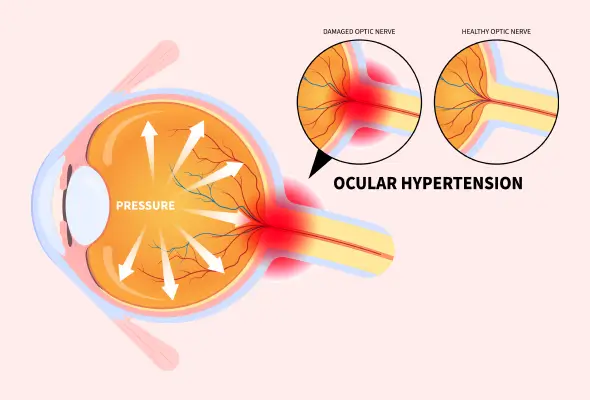
Ocular hypertension is a medical condition where the pressure in your eyes is higher than normal. This increased ocular pressure can lead to serious eye problems if left unchecked. Understanding ocular hypertension is crucial for maintaining good eye health and preventing potential vision loss.
This blog will explain the causes & symptoms of high eye pressure. We'll look at the reasons behind high pressure in your eyes, how to spot the signs, and what you can do about it.
What is Ocular Hypertension?
It occurs when the pressure inside the eye is higher than normal. The eyes constantly produce a clear fluid called aqueous humour that flows in front of the eye and then drains away. IOP increases if the aqueous humour doesn't drain out the eye when it should. This intraocular pressure (IOP) is measured in millimetres of mercury (mmHg). Typically, normal eye pressure ranges from 10 to 21 mmHg. It is considered ocular hypertension when the pressure exceeds 21 mmHg in one or both eyes at two or more check-ups.
Symptoms of Ocular Hypertension
Unlike other eye conditions that might cause discomfort or vision changes, high pressure in your eyes typically doesn't lead to any immediate or obvious signs. This silent nature of ocular hypertension means that many people are unaware they have the condition until it's diagnosed during a routine eye examination.
In rare cases, individuals with ocular hypertension might experience mild eye discomfort at touching or at movement of the eyes or headaches. However, these symptoms are not specific to ocular hypertension and could be caused by various other factors. It's important to note that blurred vision, which is often associated with eye problems, is not typically a symptom of ocular hypertension alone.

Causes of Ocular Hypertension
The primary cause of high pressure in your eyes is an imbalance in the production and drainage of aqueous humour, the clear fluid inside the eye. When the drainage channels (located in the anterior chamber angle between the iris and cornea) do not function correctly, fluid builds up, increasing intraocular pressure.
Several factors that contribute to this imbalance are:
- The drainage angle may be closed, or the drain may not drain correctly.
- A condition in which pigment particles float around the eye (Pigment dispersion syndrome) obstructs the trabecular meshwork's drainage angle.
- A condition in which protein flakes can block the drainage angle (pseudoexfoliation syndrome).
- Uveitis or inflammation of the middle portion of the eye
- Eye damage or certain eye conditions can also cause ocular hypertension.
- Eye tumour
- Large cataracts that block drainage passage
Risk Factors of Ocular Hypertension
The risk factors for developing ocular hypertension are:
- Individuals over 40 years of age are at higher risk.
- Family history and genetic factors have a significant impact on intraocular pressure.
- Ethnicity is another factor, with studies showing that African Americans and Hispanics may be at increased risk.
- Medical conditions such as diabetes, high blood pressure, and extreme nearsightedness (myopia) can also increase the likelihood of developing ocular hypertension.
- Additionally, having a thinner central cornea or bleeding at the optic nerve head may affect pressure readings and increase risk.
- Long-term use of steroid medications and a history of eye injuries or surgeries can also cause ocular hypertension.
Complications
Ocular hypertension, characterised by higher eye pressure, can lead to serious complications if left untreated. These are:
- Glaucoma
- Irreversible vision loss over time
- Retinal vein occlusion
Diagnosis of Ocular Hypertension
Diagnosing ocular hypertension involves a series of tests to measure intraocular pressure (IOP) and assess eye health.
During an eye test, the doctor will perform several investigations. These are:
- Tonometry: This test measures IOP. If initial tests show high pressure, the doctor may use more accurate tonometry, applanation tonometry, to confirm the readings. This test is considered the most accurate for measuring eye pressure.
- Optical coherence tomography (OCT): This noninvasive diagnostic test examines the optic nerve for damage or any structural abnormalities. This may require dilating the pupils. Pictures of the optic disc (the front surface of the optic nerve) are often taken for future reference and comparison.
- Visual Field Test: Also known as perimetry, a visual field test helps to check peripheral vision. This test helps detect any signs of vision loss that could indicate the development of glaucoma.
- Gonioscopy: This diagnostic test examines the drainage angle of the eye.
- Pachymetry: This critical test measures corneal thickness using an ultrasound probe, which helps determine the accuracy of IOP readings, as corneal thickness can affect pressure measurements.

Treatment for Ocular Hypertension
- Eye Drops: The most common treatment modality involves the use of prescription eye drops. These medications work by reducing fluid production in the eye or increasing its drainage, thus lowering intraocular pressure. Some of the eye drops are:
- Prostaglandin Analogues: These are typically used once a day and significantly impact lowering eye pressure.
- Beta-blockers: They can be used once or twice daily to decrease fluid production in the eye.
- Alpha-adrenergic Agonists or Carbonic Anhydrase Inhibitors: These medications can be used two to three times a day and work by reducing fluid output or increasing fluid drainage from the eye.
- Surgery: If eye drops alone don't sufficiently lower the pressure in your eyes, your doctor might recommend laser treatment or surgery. These procedures improve fluid drainage from the eye, further reducing intraocular pressure. However, these options are typically considered when medication hasn't been effective in managing the condition.

When to See a Doctor
It is recommended to have an eye test regularly if you're at higher risk of developing glaucoma. Early diagnosis & treatment of ocular hypertension can help prevent the condition from progressing to glaucoma, which is one of the major causes of permanent loss of vision if left untreated.
Seek immediate medical attention if you experience:
- Halos around lights
- Blurred vision
- Eye pain
- Any new or worsening eye-related symptoms
Prevention
While it's not always possible to prevent ocular hypertension, there are steps you can take to reduce your risk & maintain good eye health, such as:
- Regular Eye Exams: It's recommended to have an eye test at least every two years or more frequently if you're at higher risk of developing glaucoma.
- Maintaining a Healthy Lifestyle: This includes not smoking, as smoking is injurious to your overall health, including your eyes.
- Protecting Your Eyes from Potential Damage: Wear sunglasses outdoors & use protective eyewear during activities that elevate your risk of eye injury (contact sports or working with hazardous materials).
- Healthy Diet: Include dark green leafy vegetables, foods rich in vitamins C and E, and fish high in omega-3 fatty acids in your meals.
- Regular Exercise: It can also help maintain overall health and reduce eye pressure.
- Family History: Be aware of your family history of eye diseases, as some conditions, like glaucoma, can have a genetic component.
Conclusion
Taking care of your eyes includes more than just addressing ocular hypertension. It includes adopting a healthy lifestyle, protecting your eyes from damage, and being aware of risk factors. Remember, while ocular hypertension doesn't always lead to glaucoma, it's a significant risk factor that needs close monitoring. By working closely with your ophthalmologist and following their advice, you can help ensure the long-term health of your eyes.
FAQs
1. Is ocular hypertension different from glaucoma?
Ocular hypertension is indeed different from glaucoma. Ocular hypertension simply means a raised fluid pressure within the eyes, although the eyes are otherwise healthy. In glaucoma, there is usually high intraocular pressure alongside a damaged optic nerve & visual field loss. Individuals with ocular hypertension are at increased risk of developing glaucoma, but having ocular hypertension does not mean your vision is automatically at risk.
2. How can I reduce eye pressure?
To reduce eye pressure, several steps can be taken. Regular exercise can result in the lowering of intraocular pressure, and this effect can last several months. Maintaining an optimal body weight is of utmost importance, as both low and high BMI have been associated with increased risk of glaucoma condition. Sleeping with the head elevated at 20 degrees may decrease eye pressure overnight. Additionally, managing stress through practises like meditation may help reduce eye pressure.
3. What foods raise eye pressure?
While there's no direct evidence of specific foods raising eye pressure, certain dietary habits may influence ocular hypertension. Caffeine can cause a rise in eye pressure that lasts for at least 90 minutes, so moderation in caffeine consumption is advised. High intake of saturated and trans fats should be limited or avoided as they can result in weight gain and increased BMI, which may indirectly affect eye pressure. Excessive salt intake can also indirectly impact eye pressure by raising blood pressure.
4. Can lack of sleep or poor sleep cause high eye pressure?
Research indicates that sleep issues can be a contributing factor to glaucoma progression. Studies suggest that poor sleep—including sleep duration, sleep disorders, sleep disturbances, and daytime drowsiness—could be either a risk factor or a result of glaucoma. There's also a connection between glaucoma and pronounced daytime sleepiness. Untreated obstructive sleep apnea (OSA) may elevate the chance of developing glaucoma.
To Book an Appointment, call:
Still Have a Question?




