-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Glaucoma
Symptom, Causes, Diagnosis and Treatment
Glaucoma
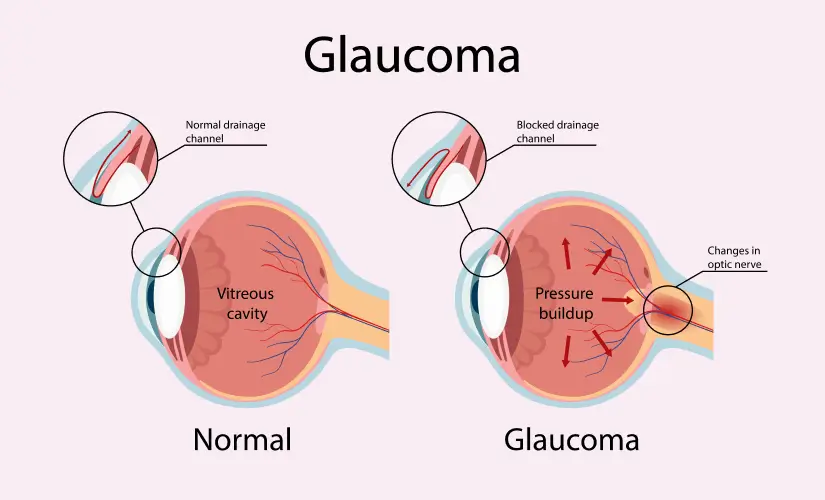
Glaucoma, a silent thief of sight, is a group of eye diseases and is a leading cause of irreversible blindness worldwide. Increased intraocular pressure contributes to optic nerve damage, impacting peripheral vision initially and progressing to central vision loss if left untreated. This condition is often famous as the "sneak thief of sight" because it advances gradually without any notice or noticeable symptoms in its early stages. However, with diagnosis at an early stage and proper treatment, you can take control and slow or even halt glaucoma progression, preserving your precious vision.
What is Glaucoma?
Glaucoma is a complex eye condition characterised by increased pressure within the eye. This pressure inside the eye is known as intraocular pressure (IOP). This increased IOP can damage the optic nerve, the main nerve responsible for transmitting visual information from the eye to the brain. If left untreated, glaucoma can cause progressive and irreversible vision loss, ultimately resulting in blindness. This underscores the significance of early detection and treatment.
The eye continuously produces a clear fluid called aqueous humour, which nourishes and maintains its proper shape. This fluid flows through a trabecular meshwork drainage system in a healthy eye, allowing for a balanced intraocular pressure. However, in people with glaucoma, this drainage system becomes compromised, leading to a buildup of fluid and increased pressure within the eye.
Glaucoma Symptoms
In the early stages of glaucoma, there are often no obvious symptoms, making it challenging to detect without regular eye examinations. As the condition progresses, symptoms may include:
- Gradual loss of peripheral (side) vision
- Tunnel vision (narrowed field of vision)
- Eye redness or pain
- Halos or rainbow-coloured rings around lights Nausea or vomiting (in cases of acute angle-closure glaucoma)
What Causes Glaucoma?
Glaucoma is caused by an imbalance between the synthesis and drainage of aqueous humour, leading to increased intraocular pressure (IOP). Over time, this increased IOP can damage the optic nerve, resulting in vision loss.
Several factors can contribute to the glaucoma, including:
- Age: The possibility of developing glaucoma increases as individuals grow older.
- Family history: Individuals with a family history of glaucoma have a higher tendency to develop the condition.
- Medical conditions: Certain medical illnesses, such as diabetes, high blood pressure, and eye injuries, can increase the chance of glaucoma.
- Ethnicity: Individuals of African, Hispanic, or Asian descent have a higher possibility of developing certain types of glaucoma.
- Corticosteroid medications: Long-term use of corticosteroids, either orally or through eye drops, can increase the risk of glaucoma.
Types
There are several types of glaucoma, each with unique characteristics and underlying causes. The two main types are:
- Open-angle glaucoma: This is the most common form of glaucoma, accounting for roughly 90% of cases. In open-angle glaucoma, the drainage angle (trabecular meshwork) remains open, but fluid drainage is impaired, leading to a gradual buildup of pressure within the eye.
- Angle-closure glaucoma: This type of glaucoma develops when there is blockage in the drainage angle between the iris and cornea, preventing the outflow of aqueous humour. This blockage can lead to a sudden and severe increase in intraocular pressure, resulting in acute angle-closure glaucoma, which is a medical emergency.
Other less common types of glaucoma include:
- Congenital glaucoma- present at birth
- Secondary glaucoma- developed from other eye conditions or medications
- Normal-tension glaucoma- optic nerve damage despite normal intraocular pressure
Glaucoma Diagnosis
Early detection and diagnosis of glaucoma are crucial steps for preserving vision and preventing further damage to the optic nerve. Comprehensive eye examinations, including the following tests, are used to diagnose glaucoma:
- Visual field test: This test evaluates peripheral vision by measuring the patient's ability to detect light in different areas of their field of vision.
- Tonometry: This test uses specialised instruments to measure the eye's intraocular pressure (IOP).
- Optic nerve examination: An ophthalmologist or optometrist will assess the optic nerve for signs of thinning or damage, which can indicate glaucoma.
- Gonioscopy: This procedure involves using a specialised lens to evaluate the eye's drainage angle, helping to determine the type of glaucoma present.
- Imaging tests: Advanced imaging techniques can provide detailed images of the retinal nerve fibre layer and optic nerve. These tests include optical coherence tomography (OCT) and scanning laser ophthalmoscopy, which aids in diagnosing and monitoring glaucoma.
Early detection and regular follow-up examinations are crucial for managing glaucoma and preventing vision loss.
Glaucoma Treatment
While glaucoma cannot be cured, various treatment approaches are available to manage the condition and slow or prevent further vision loss. The primary purpose of treatment is to lower the intraocular pressure (IOP) to a safe level, thereby reducing the chance of optic nerve damage.
Treatment options for glaucoma are:
- Eye drops: Prescription eye drops are the first line of treatment for glaucoma. These medicines either lower aqueous humour secretion or increase its drainage from the eye, effectively diminishing intraocular pressure.
- Oral medications: In some cases, ophthalmologists may prescribe oral medicines to complement eye drops or as an alternative treatment option.
- Laser treatment: Laser procedures, such as selective laser trabeculoplasty (SLT) or argon laser trabeculoplasty (ALT), can improve fluid drainage and lower IOP.
- Glaucoma Surgery: In cases where medications and laser treatments are ineffective or not well-tolerated, ophthalmologists may recommend glaucoma surgery. These procedures, such as trabeculectomy or glaucoma drainage devices, create an alternative pathway for fluid drainage from the eye, reducing intraocular pressure.
When to see a doctor
If you experience any of the following symptoms, it is essential to seek medical attention from an ophthalmologist or eye care professional:
- Sudden loss of vision or blurred vision
- Severe eye pain or redness
- Halos or rainbow-coloured rings around lights
- Nausea or vomiting (in cases of acute angle-closure glaucoma)
Additionally, doctors recommend to have regular comprehensive eye assessments, particularly if you have risk factors for glaucoma, such as:
- Age (over 60 years old)
- Family history of glaucoma
- Certain medical conditions (e.g., diabetes, high blood pressure)
- Previous eye injuries or surgeries
- Use of corticosteroid medications
Risk Factors
While glaucoma can affect anyone, certain factors can enhance an individual's risk of developing the condition. Some of the key risk factors for glaucoma are:
- Age: The risk of developing glaucoma increases significantly with age, especially after the age of 60.
- Family history: People with a family history of glaucoma have a higher chance of developing the condition, as genetic factors play a role.
- Ethnicity: Certain ethnic groups, such as Hispanics, African Americans, and Asians, have a higher prevalence of glaucoma compared to other populations.
- Medical conditions: Certain medical conditions, such as diabetes, hypertension, and cardiovascular diseases, can increase the chance of developing glaucoma.
- Eye injuries or surgeries: Previous eye injuries or surgeries, particularly those involving the eye's drainage system, can increase the possibility of glaucoma.
- Prolonged use of corticosteroids: Long-term use of corticosteroid medications, either orally or through eye drops, can contribute to the development of glaucoma.
- Thin corneas: Individuals with thin corneas (the clear front part of the eye) may be at a higher risk of developing glaucoma.
- High myopia (nearsightedness): Individuals with severe myopia (nearsightedness) have an increased risk of developing glaucoma.
Prevention
The following are some steps individuals can take to reduce their risk and maintain healthy vision:
- Regular eye examinations: Scheduling regular comprehensive eye examinations with an ophthalmologist or optometrist is pivotal for early detection and monitoring of glaucoma. An early diagnosis can prevent or slow the progression of vision loss.
- Manage underlying medical conditions: Controlling underlying systemic conditions, such as hypertension and diabetes, can reduce the risk of developing glaucoma.
- Exercise and a healthy lifestyle: Regular physical activities and a healthy, balanced diet rich in antioxidants, vitamins, and essential nutrients can support overall eye health and potentially reduce the risk of glaucoma.
- Wear protective eyewear: Protecting your eyes from potential injuries by wearing appropriate protective eyewear during sports, work, or other activities. can help prevent eye trauma, which is a risk factor for glaucoma.
- Avoid excessive alcohol intake and smoking: These habits have been correlated with an increased likelihood of developing glaucoma and other eye diseases.
- Manage eye pressure: If you have elevated IOP, following your eye care professional's recommendations for managing eye pressure through medications, lifestyle changes, or other treatments can help prevent or slow glaucoma progression.
Conclusion
Glaucoma is a progressive eye ailment characterised by optic nerve damage, often resulting from increased intraocular pressure. If left untreated, it can result in irreversible vision loss and blindness. Therefore, early detection and proper management are vital for preserving vision. Regular comprehensive eye examinations, particularly for individuals with risk factors, are essential for detecting glaucoma in its early stages. Various treatment approaches, including eye drops, laser, and surgical interventions, can effectively manage the condition and slow its progression.
FAQ's
1. How common is glaucoma?
Glaucoma is a prevalent eye illness affecting millions of people worldwide. The World Health Organisation (WHO) identifies glaucoma as the second leading reason of blindness globally. An estimated 80 million people worldwide live with the condition, with approximately 11 million experiencing bilateral blindness as a
result.
2. Can glaucoma be cured?
Unfortunately, glaucoma cannot be cured; treatment effectively manages it. Seeking timely medical intervention ensures accurate diagnosis and appropriate management initiation, helping control the condition and preserve vision.
3. What are the first signs that glaucoma is developing?
In the early stages of glaucoma, there are often no noticeable symptoms, making it challenging to detect without regular eye examinations. However, as the condition progresses, some of the first signs that glaucoma may be developing include:
- Gradual loss of peripheral (side) vision
- Narrowed field of vision (Tunnel vision)
- Eye redness or pain
- Halos or rainbow-coloured rings around lights

Still Have a Question?



