-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Celiac Disease (Gluten Intolerance)
Symptom, Causes, Diagnosis and Treatment
Celiac Disease
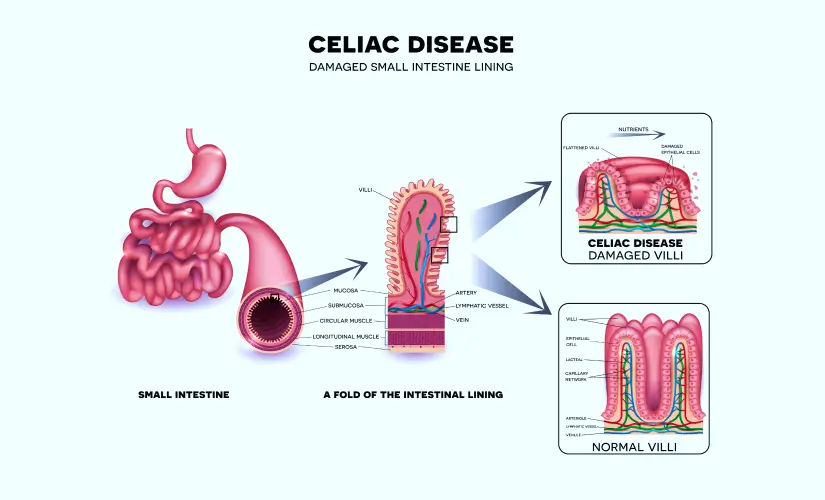
Celiac disease, commonly referred to as gluten intolerance, is a chronic autoimmune disorder affecting a person's small intestine. The main trigger is gluten consumption, a protein found in wheat, barley, and rye grains. When people with the condition consume gluten, their immune system reacts abnormally, causing inflammation and damage to the small intestine's lining. This condition can lead to various gastrointestinal symptoms. If left untreated, celiac disease in the affected person can result in severe complications. Celiac disease can profoundly impact daily life, as sticking to a gluten-free diet is crucial, making social events and eating out more difficult due to dietary limitations. Emotional strain from managing a chronic condition and potential nutrient deficiencies further exacerbates the burden.
What Causes Celiac Disease?
Various genetic and environmental factors together can cause celiac disease. The primary trigger is gluten consumption, a protein present in many whole grains, such as wheat, rye, and barley.
In people with celiac disease, the immune system reacts abnormally to gluten, causing an autoimmune response that damages the small intestine's lining.
Environmental factors, such as viral infections, severe emotional stress, or other triggers, may also activate the immune system. While infant-feeding practices, gastrointestinal infections, and gut bacteria are suspected to contribute, researchers have not definitively proven their direct causative role in celiac disease.
Symptoms of Celiac Disease
The symptoms of celiac disease can differ across the demographies and can range from mild to severe. The following are some common symptoms:
- Abdominal pain, bloating, and gas
- Diarrhoea or constipation
- Foul-smelling faeces
- Nausea and vomiting
- Weight loss and failure to gain weight
- Fatigue and weakness
Other non-gastrointestinal symptoms include:
- Anaemia (low iron levels) is due to decreased iron absorption from the small intestine
- Fatigue
- Headache
- Bone and joint pain
- Reduced bone density or softening of bone
- Skin rash or dermatitis herpetiformis
- Mouth ulcers
- Increased liver enzymes
- Neurological manifestations, such as numbness and tingling in the feet and hands, cognitive impairment, learning disabilities, lack of muscle coordination, and seizures
- Reproductive manifestations, such as delayed puberty, early menopause, or problems getting pregnant
It's important to note that some people with celiac disease may not experience any digestive symptoms, making the condition more difficult to diagnose.
Risk Factors
Several factors can increase an individual's risk of developing celiac disease, including:
- Family history: Having a first-degree relative (parent, sibling, or child) with celiac disease increases the risk.
- Genetics: Certain genetic markers, such as the HLA-DQ2 and HLA-DQ8 genes, are linked with an increased risk of developing this condition.
- Autoimmune disorders: People with other autoimmune conditions, such as autoimmune thyroiditis and hepatitis, type 1 diabetes, Sjögren's syndrome and IgA nephropathy (IgAN), have a higher possibility of developing celiac disease.
- Age: Celiac disease can develop across any age group, but it is more commonly diagnosed in early childhood or adulthood.
- Gender: Women are slightly more prone to develop celiac disease than men.
- Other genetic conditions: People with other disorders, such as Williams syndrome, Down syndrome, or Turner syndrome, have a higher tendency to develop celiac disease.
Complications
An untreated celiac disease can lead to various complications, including:
- Malnutrition: Due to the impaired absorption of nutrients, individuals with untreated celiac disease may experience malnutrition, leading to weight loss, anaemia, and other nutritional deficiencies.
- Osteoporosis: The decreased absorption of calcium and vitamin D can result in a loss of bone density and an increased risk of osteoporosis.
- Infertility: Celiac disease has been associated with an increased possibility of infertility in both men and women.
- Neurological problems: Untreated celiac disease can cause neurological issues, such as seizures, peripheral neuropathy, and ataxia (lack of coordination).
- Development of other intolerances: Chronic inflammation of the small intestine sometimes increases the possibility of developing other food intolerances, such as lactose intolerance.
- Increased risk of other autoimmune disorders: Individuals with celiac disease have a higher tendency to develop other autoimmune conditions, such as thyroid disorders or type 1 diabetes.
- Intestinal cancers: Prolonged inflammation and damage to the small intestine can increase the risk of developing certain types of intestinal cancers, such as lymphoma or adenocarcinoma.
- Liver diseases: Continuously increasing levels of liver enzymes can result in the development of various liver ailments.
Diagnosis of Celiac Disease
Diagnosing celiac disease includes a combination of blood tests, endoscopic procedures, and a thorough medical history and physical examination. The diagnostic process may include:
- Blood tests: Screening for specific antibodies, such as anti-tissue transglutaminase (tTG) and anti-endomysial antibodies (EMA), can help detect celiac disease. However, these tests alone cannot confirm the diagnosis.
- Endoscopy and biopsy: Doctors may perform an endoscopic procedure, an upper endoscopy, to obtain small tissue samples (biopsies) from the small intestine. These biopsies are then examined under a microscope for signs of damage and inflammation characteristic of celiac disease.
- Genetic testing: Genetic testing for the HLA-DQ2 and HLA-DQ8 genes can help determine if an individual has a genetic predisposition for celiac disease.
- Elimination diet: Sometimes, your doctor may recommend a gluten-free diet to observe if symptoms improve, which can help support the diagnosis.
It's essential to note that a definitive diagnosis of celiac disease requires a combination of positive blood tests, characteristic intestinal damage observed through a biopsy, and symptom improvement upon following a gluten-free diet.
Treatment
The most effective celiac disease treatment is a strict gluten-free diet followed throughout life. This involves eliminating all sources of gluten, including wheat, barley, and rye. Strict adherence to a gluten-free diet plan can help alleviate symptoms, promote healing of the small intestine, and prevent further complications.
In addition to a gluten-free meal, people with celiac disease may require nutritional supplements to address any deficiencies caused by malabsorption. Other supportive treatments may include:
- Enzyme supplements: These can help improve digestion and nutrient absorption.
- Medications: Sometimes, doctors may prescribe medicines to manage specific symptoms or complications of celiac disease.
- Counselling and support: Adopting a gluten-free lifestyle can be challenging, and counselling or support groups can help individuals cope with dietary changes and manage the emotional impact of the condition.
When to see a doctor
If you experience persistent gastrointestinal manifestations, such as abdominal pain, diarrhoea, or unexplained weight loss, it's essential to consult your doctor. Additionally, if you have a family history of celiac disease or other autoimmune disorders, you should inform your doctor about the risk factors.
Diagnosing and treating the condition promptly is essential to prevent systemic complications and promote overall health and well-being.
FAQs
1. How does celiac disease affect my body?
Celiac disease is an autoimmune disorder that activates the immune system to attack and injure the small intestine lining. This results in inflammation and interference with nutrient absorption. Left untreated, this damage can cause essential nutrient malabsorption, resulting in gastrointestinal symptoms and potential complications.
2. Is celiac disease serious?
Yes, celiac disease is a serious condition that requires ongoing management through a strict gluten-free diet. Untreated celiac disease can cause severe complications, including malnutrition, osteoporosis, infertility, neurological problems, liver diseases, and an increased possibility of certain types of cancer.
3. What foods trigger celiac disease symptoms?
The primary trigger for celiac disease symptoms is the consumption of gluten-rich food products, including wheat, barley, and rye. Food products that contain these grains, such as bread, pasta, cereals, and baked goods, can cause an immune reaction and damage the small intestine in individuals with celiac disease.
4. Can celiac go away?
Celiac disease is a life-long autoimmune disorder that does not go away on its own. However, following a strict gluten-free diet can alleviate symptoms, reduce small intestine inflammation, and prevent further complications.
5. What foods cause celiac disease?
Any specific food does not cause celiac disease. Instead, it is triggered by gluten consumption, a protein found in wheat, barley, and rye. Foods containing these grains, such as bread, pasta, cereals, and baked goods, can trigger an immune reaction and damage the small intestine in individuals with celiac disease.

Still Have a Question?



