-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Black Fungus
Symptom, Causes, Diagnosis and Treatment
Black Fungus
Infection with black fungus or mucormycosis is uncommon yet dangerous. The infection is more common in those who have impaired immune systems or who take excessive amounts of steroid medicines. A black fungal infection carries a high risk of death and can result in life-threatening consequences if not treated promptly. It is caused by a group of molds called mucormyocetes and enters the body through the inhalation of spores. It can spread to any part of the body and is then called Disseminated mucormycosis
What is Black Fungus?
Black fungal infection, commonly referred to as mucormycosis, is an uncommon but harmful condition. It is caused by molds known as mucormycetes, which usually affect the sinuses, lungs, skin, and brain. Exposure to mold spores can occur through inhalation or contact with infected soil, rotting bread, or vegetables, compost piles, or other objects.
What are the symptoms of Black fungus (Mucormycosis)?
Black fungus symptoms manifest depending on where they grow, in the skin, brain or respiratory system. The following black fungus symptoms could indicate an upper or lower respiratory illness
- Cough
- Nasal obstruction
- Fever
- Headache
- Chest pain
- Breathing difficulty or breathlessness
- Black lesions on the nasal bridge or inside the oral cavity
Mucormycosis can appear anywhere on the body as a skin infection. It may initially cause skin damage but can swiftly spread to other areas. Symptoms of black fungus on the skin include:
- Blisters
- Ulcers
- Fever
- Oedema
- Redness
- Darkened skin tissue
- Blackened boils
- Painful lesions
The black fungus can also affect the eyes. Here are some starting symptoms of black fungus in eyes:
- Blurred vision
- Blood clots
- Double vision
- Teariness
- Headache
- Malaise
- Congestion
- Blood-tinged secretions
The black fungus can affect the digestive system
- Diarrhoea
- Bloody stools
- Nausea and vomiting
- Vomiting blood
- Pain abdomen
What are the causes of Black fungus (Mucormycosis)?
Exposure to black fungus molds is one of the main causes of black fungus. These microbes are found in leaves, compost piles, soil, and rotting wood, stale bread, and veggies. Inhaling airborne mold spores from an infected area can cause mucormycosis, As a result, the following areas might be affected:
- Eyes
- Face
- Lungs
- Sinuses
- Skin
- Central nervous system (less frequently)
Additionally, a cut or burn to the skin can expose a person to the fungus (cutaneous exposure). In these situations, the burn or wound ultimately becomes infected. Although many molds can exist in the environment naturally, not everyone who is exposed will develop a fungal infection. If the immune system is compromised, a person may be more likely to have this kind of infection. The following health conditions might increase the chances of getting the fungus:
- Cancer
- Burns
- HIV/AIDS
- People on immunosuppressants
- Uncontrolled diabetes
- Recent organ transplant
- Stem cell transplant
- Neutropenia
- Chemotherapy
- Long-term steroid use
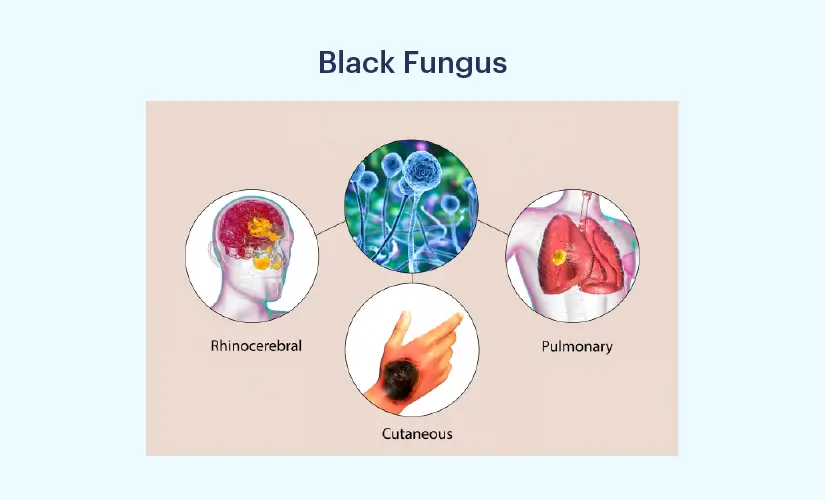
What are the types of Black fungus disease Mucormycosis)?
Mucormycosis is classified into the following categories, depending on the body part it affects:
- Rhinocerebral: Affects the sinuses and brain
- Pulmonary: Affects the lungs
- Cutaneous: Affects the skin
- Gastrointestinal: Affects the stomach and gut
- Disseminated: Affects multiple body parts, such as the lungs, skin, sinuses, brain, inner lining of the heart chambers, heart valves, and kidneys
Risk Factors of Black Fungus
Preventing this rare infection is crucial for individuals with compromised immune systems, which can result from conditions such as diabetes, cancer, organ or stem cell transplants, neutropenia, prolonged corticosteroid use, injection drug use, iron overload, or skin injuries from surgery, burns, or wounds. It is essential to take preventive measures to avoid the occurrence of this infection in immunocompromised individuals.
Prevention of Black Fungus
Preventing black fungus, also known as mucormycosis, involves several key measures:
- Control Diabetes: Since uncontrolled diabetes is a significant risk factor, maintaining blood sugar levels within the normal range is crucial. Regular monitoring and adherence to a diabetes management plan are essential.
- Sterile Medical Procedures: Ensuring strict hygiene during medical interventions, especially surgeries, and maintaining a sterile environment can help prevent fungal infections.
- Proper Steroid Use: If corticosteroids are necessary, they should be prescribed and used under medical supervision. Dosage and duration should be carefully monitored to prevent overuse.
- Aseptic Wound Care: For individuals with skin injuries due to surgery, burns, or wounds, proper and aseptic wound care is essential to prevent fungal contamination.
- Personal Hygiene: Maintaining good personal hygiene, including regular handwashing, can help reduce the risk of fungal infections.
- Iron Management: In cases where iron overload or hemochromatosis is a concern, managing iron levels through medical guidance is important to prevent complications.
- Immune System Support: Boosting and maintaining a healthy immune system is crucial. This can include a balanced diet, regular exercise, adequate sleep, and, in some cases, immunization against certain diseases.
Treatment options for Mucormycosis
Before starting black fungus treatment, the doctor will conduct a physical examination and inquire about the patient's medical history if they suspect mucormycosis. It is important to inform the doctor if the patient has been around stale food or other areas where fungal spores are commonly found. This is typically done to eliminate any other possible conditions. The following diagnostic tests may be ordered by the doctor:
- The most common presenting symptom for clinical diagnosis is a headache. Tissue necrosis is also a sign of black fungus infection, which can be detected by looking for eschar (a black scab) in the mouth or nasal cavity. The presence of eye redness, protrusion, swelling, loss of vision, intense facial pain, and localized numbness should raise suspicion of the condition.
- Imaging techniques such as a CT scan of the brain and paranasal sinuses help in detecting rhino-orbital disease.
- Histopathological and microbiological examinations are performed to identify the fungus in the tissues.
- Microscopic examination of the tissue to identify the fungus and check for the uptake of specific stains is a crucial step in the diagnosis, according to histopathological and microbiological examination.
- Molecular assays, such as DNA sequencing of specific gene regions, melt curve analysis of PCR products, conventional polymerase chain reaction (PCR), and restriction fragment length polymorphism analyses (RFLP), can be used to detect Mucorales, the pathogen responsible for black fungus disease. However, these tests are rarely performed since a microscopic examination is usually sufficient.
If mucormycosis is diagnosed, the doctor may prescribe immediate treatment for black fungal infection, which typically involves antifungal drugs administered through intravenous (IV) or oral pills. These medications aim to eliminate the fungus, inhibit its growth, and control the infection. In the initial stages, the doctor may administer high doses intravenously until the infection is brought under control. If the prescribed drug causes uncomfortable side effects such as heartburn or stomach pain, it is important to inform the doctor so that they can adjust the medication or dosage accordingly.
Though there are various home remedies for black fungus treatment at home, they can only help you to alleviate the symptoms and boost the immune system.
When to visit a doctor for black fungal infections?
If the symptoms do not improve or persist, it is important to seek medical attention. A doctor will diagnose and treat the condition, prescribing appropriate antibacterial and antifungal drugs.
Conclusion
Early diagnosis and therapy are crucial for a successful recovery from mucormycosis. There is a risk that the infection may spread to other parts of the body, and in severe cases, it can lead to death. Therefore, it is important to treat mucormycosis promptly to prevent any complications. While mucormycosis is not common, it must be treated as soon as possible to avoid the development of other associated conditions. To rule out any underlying causes or additional infections related to black fungus, the doctor thoroughly examines the patient.
FAQs
1. Is black fungal disease (mucormycosis) deadly?
Black fungal disease, also known as mucormycosis, is a severe infection that can be life-threatening if not treated in a timely manner. Therefore, if someone experiences symptoms such as nasal obstruction, fever, or flu-like symptoms, it is important to seek medical attention.
2. How long does mucormycosis treatment take?
Based on current studies and observations, it took a patient 102 days to recover from primary mucormycosis and 33 days from refractory mucormycosis.
3. Can black fungus make you sick?
Black fungus is generally not harmful, but it can cause serious illness in individuals with weakened immune systems or other medical conditions such as diabetes, HIV, or AIDS.
4. What is the best medicine for black fungus?
Doctors typically prescribe antifungal medications, along with some vaccines, to treat black fungus. Additionally, there are certain home remedies that can help patients feel better.
5. What happens if I leave black fungus untreated?
If left untreated, the condition can worsen and may even result in the death of the patient. Therefore, it is advisable to consult a doctor for proper treatment and recovery.

Still Have a Question?



