Septate Uterus
Many women discover they have a septate uterus only after experiencing pregnancy complications or multiple miscarriages. This common uterine abnormality affects about 1 in every 200 women worldwide. This comprehensive guide explains everything about the septate uterus - from its causes and symptoms to diagnosis methods and treatment approaches.
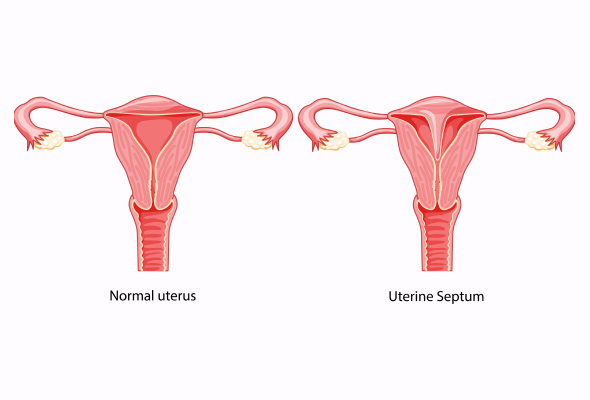
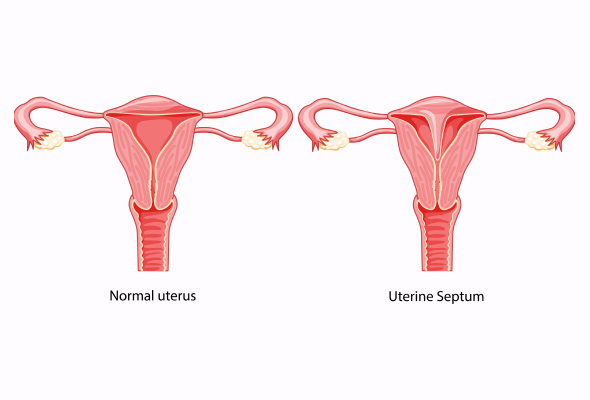
What is a Septate Uterus?
A septate uterus is a congenital condition where a thin membrane, called the septum, divides the uterus into two separate chambers. While appearing normal from the outside, like an upside-down pear, the internal cavity is split, creating a distinctive heart-shaped structure.
This condition represents the most common uterine abnormality, accounting for approximately 55% of all uterine malformations. The septum can vary in both thickness and length, potentially extending from the top of the uterus down to the cervix.
Key characteristics of a septate uterus include:
- Normal external uterine shape
- Internal division- creating two smaller cavities
- Varying septum thickness and length
- Possible extension to the cervix and occasionally to the vagina
- It can be an incomplete (partial septate uterus) or complete division
Septate Uterus Symptoms
Many individuals may carry this condition without experiencing any noticeable signs throughout their daily lives.
However, when symptoms do appear, they typically include:
- Frequent miscarriages - Often the first indication of the condition
- Painful menstruation (dysmenorrhea)
- Persistent pelvic pain
- Unusual menstrual bleeding that may not be effectively contained by tampons
Causes of Septate Uterus
The development of a septate uterus begins long before birth, during the early stages of foetal development. This congenital condition results from an incomplete fusion of the Müllerian ducts, which are essential structures in female reproductive development.
The formation process occurs around the seventh week of embryonic development when two structures called paramesonephric ducts begin their crucial development journey. These ducts are responsible for forming the upper portion of the vagina, cervix, uterus, and fallopian tubes.
These ducts should undergo a vertical fusion by the eighth week, creating a midline septum. Usually, this septum disappears by week 20 of embryonic development through a process called resorption. However, when this resorption process is interrupted, a septate uterus develops.
Complications of Septate Uterus
The presence of a septum can lead to several pregnancy-related complications:
- Restricted foetal growth and low birth weight
- Preterm birth and premature labour
- Breech presentation requiring caesarean delivery
- Second-trimester pregnancy loss
Septate Uterus Diagnosis
Modern diagnostic approaches rely heavily on various imaging tools to accurately visualise the septum's position and thickness. The most commonly used diagnostic methods include:
- Septate Uterus Ultrasound: 3D Ultrasound is the preferred option due to its cost-effectiveness and accuracy in distinguishing between different uterine anomalies
- MRI (Magnetic Resonance Imaging): Gives detailed images of the uterine structure with 100% accuracy
- Hysteroscopy: Provides direct visualisation of the uterine cavity through a small camera
- Laparoscopy: Enables doctors to examine the external uterine structure
Septate Uterus Treatments
Treatment options for a septate uterus have evolved significantly over the years, with surgical intervention being the primary approach for those experiencing fertility challenges or recurring miscarriages.
Hysteroscopic Metroplasty: This commonly used minimally invasive outpatient procedure takes approximately one hour and involves removing the septum through the cervix, creating a single uterine cavity. Studies show that after this procedure, pregnancy rates can reach up to 65%.
The procedure offers several advantages:
- No visible incisions
- Same-day discharge
- Faster recovery period
- Reduced risk of complications
- Possibility of vaginal delivery in future pregnancies
While surgery isn't always necessary, particularly for asymptomatic women, it becomes crucial for those experiencing recurrent pregnancy losses. After surgical correction, the risk of miscarriage significantly decreases.
Pregnancy experts typically recommend waiting two months post-surgery before attempting conception.
When to See a Doctor
Women experiencing recurrent pregnancy losses should consult a fertility specialist, as a septate uterus might not be detected during routine examinations. For pregnant women with a septate uterus, certain symptoms require immediate medical attention:
- Pelvic cramping or contractions
- Rupturing of membranes
- Vaginal bleeding
- Signs of preterm labour
Prevention
While prevention isn't possible, as it is a congenital condition, women diagnosed with a septate uterus can take several steps to manage their pregnancy and reduce associated risks.
Doctors recommend several lifestyle modifications to help manage pregnancy with a septate uterus:
Conclusion
A septate uterus presents unique challenges for women during their pregnancy journey. Though this congenital condition affects many women worldwide, medical advances have made it feasible to diagnose and treat it effectively. Modern surgical techniques like hysteroscopic metroplasty offer hope to women experiencing recurring pregnancy losses.
Women diagnosed with a septate uterus should remember that successful pregnancies are possible with proper medical care. Regular check-ups, early intervention, and lifestyle modifications significantly improve pregnancy outcomes.
FAQs
1. How serious is a septate uterus?
A septate uterus requires careful medical attention due to its impact on pregnancy outcomes. Studies show that women with this condition face a miscarriage rate of about 35%. Additionally, there's a 26% to 94% chance of miscarriage for each pregnancy that develops within a septate uterus.
2. How common is a septate uterus?
This condition represents the most common uterine anomaly, accounting for approximately 55% of all uterine malformations. The prevalence is estimated to be up to 1.5% in reproductive-age females.
3. Is having a septate uterus bad?
Having a septate uterus isn't necessarily harmful to overall health, but it can affect reproductive outcomes. While some women experience no issues, others may face:
- Increased risk of miscarriage
- Higher chances of preterm delivery
- Possible complications during pregnancy
4. How does a septate uterus affect periods?
A septate uterus typically doesn't significantly impact menstruation, though some women may experience heavier bleeding due to increased endometrial surface area. Some individuals might experience menstrual pain, while others have no symptoms at all.
5. Can a septate uterus grow back?
No, once surgically removed, a septate uterus cannot grow back. The septum develops during foetal formation, and the body cannot regenerate it after surgical removal.
6. How do you increase uterus size naturally?
Several natural approaches can support uterine health:
- Maintaining a balanced diet rich in vitamins and minerals
- Regular exercise, especially pelvic-focused activities
- Adequate hydration
- Stress reduction techniques