Pericardial Effusion
A thin, double-layered sac called the pericardium protects the heart. When excess fluid builds up between these layers, doctors call this condition pericardial effusion. The pericardial effusion causes fatigue, shortness of breath, and a constant feeling of pressure, which can affect daily activities. This comprehensive guide explains everything patients need to know about pericardial effusion. You will learn about its signs and symptoms, common causes, available treatments, and when they should seek immediate medical attention.
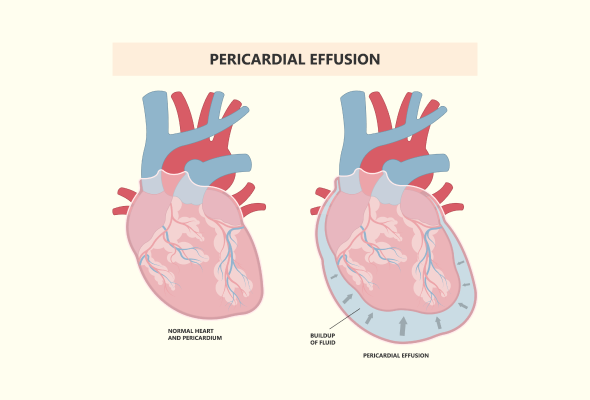
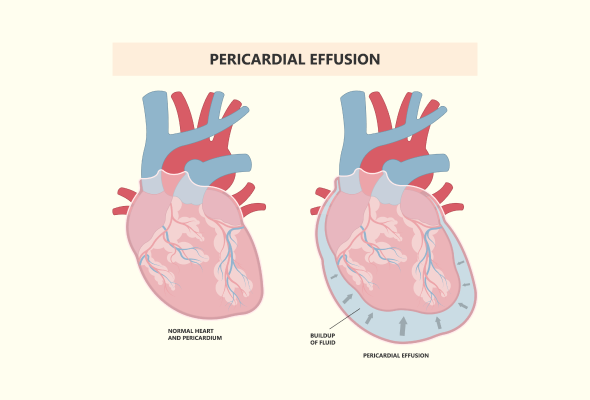
What is Pericardial Effusion?
Pericardial effusion develops when excess fluid accumulates in the space between the two layers of the pericardium, the protective sac surrounding the heart. This condition can develop either gradually or suddenly, each presenting different challenges to heart function.
When fluid builds up slowly, the pericardium has time to stretch and accommodate the extra fluid. However, a rapid accumulation can be more dangerous as the pericardial sac doesn't have sufficient time to adapt. In either case, the presence of excess fluid can significantly impact how the heart functions.
Pericardial Effusion Symptoms
Many patients experience no noticeable signs, mainly when the fluid accumulates slowly. Common pericardial effusion signs and symptoms include:
- Breathing difficulties, especially when lying down
- Chest pain or pressure, typically behind the breastbone
- Rapid heartbeat
- Lightheadedness or fainting spells
- Fatigue and weakness
- Swelling in the abdomen or legs
- Trouble swallowing
- Persistent hiccups
- Coughing or hoarseness
Causes and Risk Factors of Pericardial Effusion
The leading causes of pericardial effusion include:
- Infections: Viral and bacterial infections, including HIV and tuberculosis, can trigger fluid buildup. In developing countries, tuberculosis remains the most common cause.
- Cancer-related Issues: Both primary heart tumours and cancer that spread from other parts of the body can affect the pericardium
- Autoimmune Conditions: Disorders such as lupus, rheumatoid arthritis, and Sjögren's syndrome can lead to pericardial effusion
- Medical Procedures: Heart surgery, radiation therapy for cancer, and certain medications can cause this condition
Several underlying systemic conditions can increase the risk of developing pericardial effusion. These include:
- Heart failure
- Chronic kidney disease
- Liver cirrhosis
- Hormonal disorders, particularly an underactive thyroid (hypothyroidism)
- Chest injuries from car accidents or wounds from sharp objects
- Heart-related issues such as heart attacks, valve diseases, or aortic dissection
Complications of Pericardial Effusion
- Cardiac Tamponade: The most serious complication of pericardial effusion is cardiac tamponade, a life-threatening condition that requires immediate medical attention. This occurs when excess fluid puts pressure on the heart, preventing it from filling adequately with blood.
- Pericardial Decompression Syndrome (PDS): PDS is a rare but serious complication that can occur after draining the excess fluid. This condition is particularly concerning for patients with large effusions and underlying heart problems. PDS can cause unexpected deterioration in a patient's condition, even after what appears to be successful treatment.
Diagnosis of Pericardial Effusion
During the initial assessment, doctors listen carefully to heart sounds using a stethoscope to detect abnormalities.
Several diagnostic examinations help confirm the presence and severity of pericardial effusion:
- Echocardiogram: This primary diagnostic tool uses sound waves to create detailed heart images, showing the amount of fluid and its effect on heart function
- Electrocardiogram (ECG): This test measures the heart's electrical activity and can reveal patterns suggesting cardiac tamponade
- Chest X-ray: While less sensitive, it can show signs of an enlarged heart if the effusion is large
- Advanced Imaging: CT scans and MRI provide detailed views of the heart and can detect pericardial effusion, though they're typically used when other conditions are suspected
Treatments
The following are common pericardial effusion treatment approaches:
- Wait and Watch: Doctors may recommend monitoring the condition for mild cases without symptoms while treating the underlying cause.
- Medications:
- Anti-inflammatory drugs to reduce inflammation
- Colchicine combined with conventional therapy (This treatment approach has been shown to reduce symptoms within 72 hours in 88.3% of cases)
- Antibiotics for bacterial infections
- Corticosteroids for cases unresponsive to other treatments
- Surgical and Drainage Procedures:
- Pericardiocentesis: The most common procedure where doctors use a catheter and needle to drain excess fluid. This procedure has shown a 95% success rate
- Pericardiectomy: This procedure involves surgical removal of part or all of the pericardium when other treatments fail
- Video-assisted thoracic surgery (VATS): Creates a pericardial window to allow fluid drainage
When to See a Doctor
Immediate emergency care is essential if patients experience any of these warning signs:
- Chest pain
- Difficulty breathing or rapid breathing
- Skin turning pale, grey, or blue
- Fainting or severe dizziness
- Heart palpitations
- Resting pulse exceeding 100 beats per minute
Prevention
Doctors recommend several strategies to minimise the risk of developing pericardial effusion:
- Prompt Treatment of Infections: Addressing infections early can prevent them from affecting the heart
- Safety During Activities: Using proper protective equipment during sports and outdoor activities that carry injury risks
- Managing Underlying Conditions: Effective treatment of existing health conditions like autoimmune diseases or cancer can reduce the risk
- Radiation Therapy Monitoring: Patients receiving chest radiation should undergo regular monitoring for signs of pericardial effusion
- Regular Health Check-ups: Maintaining scheduled appointments with doctors for ongoing monitoring
- Heart-healthy Lifestyle: Following a balanced diet, regular exercise, and maintaining a healthy weight
- Alcohol Moderation: Limiting alcohol consumption to prevent heart-related complications
- Genetic Screening: Individuals with family history may benefit from genetic counselling
Conclusion
Pericardial effusion requires careful attention and prompt medical intervention when symptoms appear. Though the condition can be serious, modern medical treatments offer effective solutions, with success rates reaching 95-100%, depending on the chosen procedure. Patients who notice any warning signs should not hesitate to seek medical help. Quick action, especially when experiencing chest pain or breathing difficulties, can prevent serious complications like cardiac tamponade.
A heart-healthy lifestyle and proper management of underlying conditions give patients the best chance of preventing pericardial effusion. Regular medical check-ups, early treatment of infections, and careful monitoring of existing health conditions help reduce the risk of developing this heart condition. Patients can effectively manage pericardial effusion and maintain their heart health through proper awareness and timely medical care.
FAQs
1. How common is pericardial effusion?
Studies show that pericardial effusion affects a significant portion of the population. In Western countries, the condition has an estimated incidence of 3% and a prevalence between 5.7% and 9%. The condition can affect people of any age or background, making it a relatively common heart-related concern.
2. How long pericardial effusion lasts?
The duration of pericardial effusion varies significantly among patients. Medical records show that cases can last anywhere from 6 months to 15 years, with a median duration of 3 years. Small effusions that don't cause symptoms may persist for extended periods, while larger effusions requiring immediate treatment typically resolve more quickly with proper medical intervention.
3. What is the primary difference between cardiac tamponade and pericardial effusion?
While pericardial effusion refers to fluid accumulation around the heart, cardiac tamponade is a serious complication that can develop from it. Key differences include:
- Cardiac tamponade occurs when the fluid creates high pressure that prevents proper heart function
- In tamponade, the heart chambers collapse during diastole due to excessive pressure
- Regular pericardial effusion may be well tolerated, mainly if it develops slowly
- Tamponade requires immediate medical intervention