-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Uremia
Symptom, Causes, Diagnosis and Treatment
Uremia
Uremia is a systemic condition that occurs when the kidneys are no longer able to completely filter waste products from the blood, resulting in toxic accumulation within the body. As these waste products build up, they can disrupt many processes in your body and lead to symptoms of anaemia and other complications. Here, we will discuss all the aspects of uremia in detail.
What is Uremia?
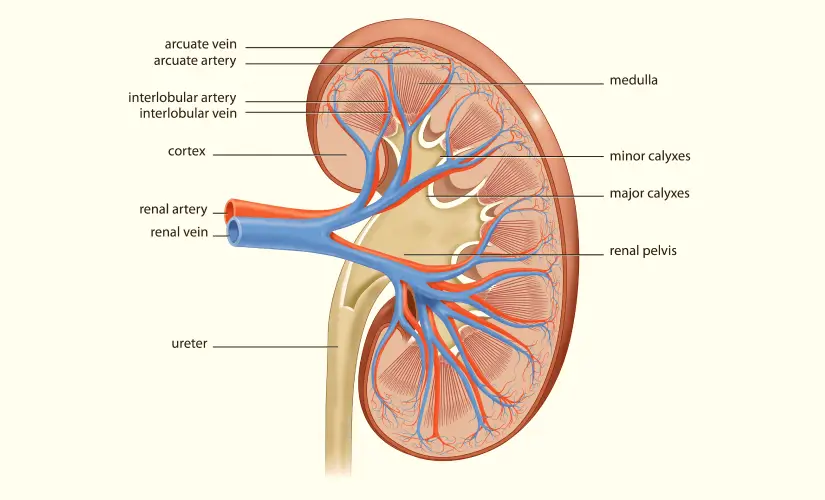
Uremia, also known as uremic syndrome or kidney failure, happens when the kidneys lose their ability to function fully. The primary objective of kidneys is to filter the blood (removing waste products, excess water, and toxic substances). However, when they fail to do so correctly, these substances build up in the blood and cause a condition known as uremia.
How Common is Uremia?
Uremia syndrome prevalence varies with age, geographic area, and co-existing conditions. The risk of uremia goes up with age and is more common in people who have high blood pressure, uncontrolled diabetes, or other chronic diseases that slowly raise the risk for kidney problems over time. Kidney disease uremia is a serious condition and, if left unattended, can be life-threatening.
Symptoms of Uremia
The uremia symptoms can range from mild to severe, based on the degree of kidney dysfunction and the concentration of waste products in your blood. Common symptoms include:
- Fatigue and severe weakness
- Nausea and vomiting
- Loss of appetite
- Itchy skin
- Swollen legs, ankles, or feet (oedema)
- Difficulty concentrating
- Shortness of breath
- Metallic taste in the mouth
- Muscle cramps or twitches
- Confusion or disorientation
Causes of Uremia
- Chronic Kidney Disease (CKD): A long-term condition where the kidneys cannot function properly due to diseases like diabetes, high blood pressure or glomerulonephritis.
- Acute Kidney Injury (AKI): AKI is the sudden loss of your kidneys' ability to perform their functions, causing uremia. Typically triggered by dehydration or infection and sometimes due to medications/chemicals.
- Obstructive Uropathy: This renal condition occurs when an obstruction or blockage in the urinary tract impedes normal urination. As a result, wastes build up inside the body, leading to uremia.
- Glomerulonephritis: This inflammatory process affects the filtering units (glomeruli) and often results in decreased kidney function.
- Polycystic kidney disease: This inherent lifelong condition can drive the development of cysts in one or both kidneys and possible progressive impairment of renal function.
Diagnosis
Diagnosing uremia involves a combination of medical history, physical examination, and laboratory tests. Your doctor may order the following tests:
- Blood Tests: Simple blood tests measure the levels of waste products like creatinine and urea nitrogen in the blood. High amounts of these substances can suggest that the kidneys cannot properly process and remove them from the blood.
- Urine Tests: Urinalysis may reveal the presence of protein, blood or other abnormalities that suggest kidney disease.
- Imaging tests: These diagnostic methods involve using ultrasound, CT scans, or MRI to examine your kidneys and check their health.
- Kidney Biopsy: During a biopsy, doctors may remove a small sample of kidney tissue and observe it under a microscope to determine the cause of an abnormal function.
Treatment for Uremia
The uremia treatment primarily depends on the underlying cause and severity of the condition. The following are some common treatment options:
- Dialysis: This is a process that filters waste products, including toxins and excess fluids, from your blood flow when your kidneys are unable to do so effectively. There are two main types of dialysis:
- Peritoneal Dialysis: This procedure involves using the lining of your abdomen (peritoneum) to filter toxins and waste products from your blood.
- Hemodialysis: This method involves using a machine to filter blood outside your body.
- Kidney Transplantation: Sometimes, for end-stage renal disease (ESRD), doctors may recommend a kidney transplant to replace the failing kidneys with a healthy, donated kidney.
- Medication: Depending on the underlying cause of uremia, your doctor may prescribe medications to manage associated conditions, such as high blood pressure, diabetes, or infections.
- Dietary Modifications: Restricting your intake of certain nutrients, such as protein, potassium, and phosphorus, can help lower the buildup of waste products in your blood.
Risk Factors
Several factors can increase the possibility of developing uremia, including:
- Diabetes: Uncontrolled high glucose levels are a leading cause of chronic kidney disease and can ultimately lead to uremia.
- High Blood Pressure: Hypertension can damage the blood vessels of the kidneys over time, increasing the risk of uremia.
- Family History: Certain inherited conditions, such as polycystic kidney disease, can increase your risk of kidney failure and uremia.
- Older Age: Kidney disease and uremia risk increases as you get older.
- Obesity: Being overweight or obese can put your kidneys under stress and contribute to the development of uremia.
- Smoking: Smoking has been correlated with an increased risk of kidney disease and uremia.
- Certain Medications: Some medications, such as certain chemotherapy drugs and non-steroidal anti-inflammatory drugs (NSAIDs), can potentially damage the kidneys if used excessively or improperly.
Complications of Uremia
If left untreated, uremia can lead to several serious complications, including:
- Fluid and Electrolyte Imbalances: The buildup of waste products in the blood can disrupt the fluid & electrolyte balance in the body, leading to conditions like oedema (swelling), muscle cramps, and irregular heartbeats.
- Cardiovascular Complications: Uremia can contribute to the development of high blood pressure, heart disease, and an increased risk of stroke.
- Bone and Mineral Disorders: The accumulation of particular waste products, such as phosphorus, can lead to bone disorders like renal osteodystrophy, which can cause bone pain, fractures, and deformities.
- Neurological Complications: Uremia can affect the brain and nervous system, resulting in symptoms like confusion, seizures, and coma.
- Anaemia: Impaired kidney function can interfere with erythropoietin synthesis, a hormone that stimulates red blood cell production, resulting in anaemia.
- Metabolic Acidosis: The acid buildup in the body due to impaired kidney function can disrupt various bodily processes and lead to complications like muscle wasting and bone loss.
Prevention
While some factors that contribute to uremia may be beyond your control, there are several steps you can take to reduce your risk:
- Manage other diseases: If you have diabetes, high blood pressure, or kidney disease, you must follow your doctor's advice to manage these treatable conditions well.
- Follow a healthy lifestyle: Eating a healthy diet, working out every day, and quitting smoking can give you first-rate protection in your kidneys.
- Drink water: Staying well-hydrated helps your kidneys work better and reduces the chances of accumulating waste products.
- Medication management: Some medications, chemicals and substances can be toxic to your kidneys, so it is better to follow your doctor's advice.
- Changes in diet: Managing the amount of protein, potassium and phosphorus you consume can limit waste product protection that builds up in your blood.
When to See a Doctor
If you experience any of the following symptoms, it's crucial to seek medical attention promptly:
- Decreased urine output or difficulty urinating
- Swollen legs, ankles, or feet
- Severe weakness
- Confusion or disorientation
- Shortness of breath
- Severe muscle cramps or twitches
Conclusion
Uremia is a systemic condition in which kidneys fail to perform their functions, such as removing toxins, waste products, and excess fluids. If left unmanaged, uremia can turn into a serious problem with implications across the body. If you know the causes, symptoms and treatment, you can proactively take measures to look after your kidneys’ health and seek help as soon as needed. Keep in mind that timely diagnosis and correct treatment may prevent or delay uremia, as well as its complications.
FAQs
1. Who is most likely to get uremia?
Individuals with diabetes, chronic kidney disease, or high BP have a higher risk of developing uremia. Older adults and those with a family history of kidney disorders are also more susceptible.
2. What is the normal range of uremia?
There is no definite uremia level. It is a condition marked by the buildup of waste products in the blood. Doctors monitor levels of substances like creatinine and blood urea nitrogen (BUN) to assess kidney function and detect uremia.
3. What stage of kidney disease is uremia?
Uremia typically occurs in the later stages of chronic kidney disease, often referred to as stage 4 or stage 5 (end-stage renal disease or ESRD). At these stages, the kidneys are functioning at less than 30% of their normal capacity, leading to waste buildup in the bloodstream.
4. Is kidney transplantation an option for treating uremia?
Yes, kidney transplantation is a treatment option for individuals with end-stage renal disease (ESRD) and uremia. A successful kidney transplant (KTP) can restore normal kidney function and exclude the need for dialysis.
5. Can kidney function improve without dialysis?
In some cases, kidney function may improve without dialysis. This depends on the cause of kidney impairment. For example, if uremia is due to acute kidney injury from dehydration or certain medications, addressing the issue can help the kidneys recover. However, in chronic kidney disease or end-stage renal disease (ESRD), dialysis or a kidney transplant (KTP) is often necessary to manage uremia effectively.
To Book an Appointment, call:
Still Have a Question?




