-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Sarcoidosis
Symptom, Causes, Diagnosis and Treatment
Sarcoidosis
Sarcoidosis affects lakhs of people worldwide, yet many have never heard of this inflammatory disease. This condition occurs when clusters of inflammatory cells form in different organs throughout the body. While some might worry that sarcoidosis is cancer, it is actually a different type of condition that requires a specific treatment approach. This comprehensive guide explains sarcoidosis, including its symptoms, causes, diagnosis, and treatment options.
What is Sarcoidosis?
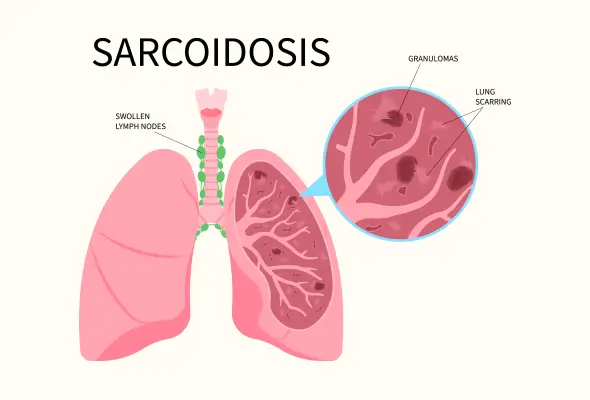
Sarcoidosis is a complex inflammatory disease where the body's immune system forms tiny clusters of cells called granulomas in various organs. These granulomas are the body's defensive response, creating small inflammatory cell lumps that can develop in any part of the body.
While sarcoidosis can affect multiple organs simultaneously, it most commonly appears in:
- Lungs and chest lymph nodes
- Skin and eyes
- Heart and other organs
- Muscles and joints
- Liver and spleen
Sarcoidosis Symptoms
The symptoms of sarcoidosis vary significantly depending on which organs the inflammatory granulomas affect and the size of the granulomas.
- General Sarcoidosis Disease Symptoms:
- Persistent fatigue
- Unexplained weight loss
- Swollen lymph nodes
- Joint pain and swelling
- Night sweats
- Muscle weakness
- Lung Symptoms: When sarcoidosis of the lung do appear, it may cause the following:
- Persistent Dry Cough
- Shortness Of Breath
- Chest Discomfort
- Wheezing, particularly during physical activity
- Skin Symptoms:
- Reddish-purple bumps on the shins or ankles
- Disfiguring sores on the nose, cheeks, or ears
- Darker or lighter patches of skin
- Eye Symptoms: Eye problems can develop without initial symptoms, making regular eye examinations crucial. When symptoms do appear, they often include:
- Blurred vision
- Eye pain
- Increased sensitivity to light
- Burning or itching sensations and severe redness
- Heart-related Symptoms:
- Irregular heartbeats
- Chest pain
- Shortness of breath
- Fainting spells or heart palpitations
- Swelling in the legs, which is a result of fluid retention
Sarcoidosis Causes
The disease develops when the body's immune system responds unusually to specific triggers, causing inflammation to go off track.
The development of sarcoidosis stems from a perfect storm of various factors. When specific environmental triggers encounter a person's genetic predisposition, the immune system can overreact, forming granulomas in different organs.
The following are some common sarcoidosis reasons:
- Environmental Exposures: Contact with insecticides, mould, or industrial materials, particularly affecting healthcare workers, automotive industry workers, and firefighters
- Infectious Agents: Exposure to certain bacteria or viruses
- Genetic Factors: Having specific genes that affect immune system responses
- Occupational Risks: Working in environments with exposure to dust, chemicals, or other inflammatory substances
- Medical Treatments: Certain HIV medicines and specific cancer treatments
Key risk factors for developing sarcoidosis include:
- Age: Most cases occur between ages 20 and 60, with increased risk after age 55
- Gender: Women show slightly higher susceptibility than men
- Race and Ethnicity: People of African descent and Northern European (particularly Scandinavian) heritage face higher risks
Complications of Sarcoidosis
The most serious complications can affect various organs:
- Lungs: Untreated pulmonary sarcoidosis can cause permanent scarring (pulmonary fibrosis), making breathing difficult. This scarring may lead to pulmonary hypertension, forcing the heart to work harder to supply blood through damaged lung vessels.
- Eyes: Inflammation can damage the retina and potentially cause blindness. Some patients develop cataracts or glaucoma, requiring immediate medical intervention.
- Kidneys: The disease can disrupt calcium handling in the body, leading to kidney stones and reduced kidney function. In severe cases, this might progress to kidney failure.
- Heart: Cardiac sarcoidosis creates granulomas in heart tissue that can disturb normal heart rhythm and blood flow. This serious complication requires careful monitoring as it can be life-threatening.
- Nervous System: When granulomas develop in the brain & spinal cord, patients may experience facial paralysis, seizures, or symptoms similar to multiple sclerosis.
Diagnosis
- Physical Evaluation: Firstly, doctors assess symptoms and listen carefully to the patient's heart and lungs. Doctors also check for swollen lymph nodes and examine any skin lesions that might be present.
To confirm a sarcoidosis diagnosis, doctors rely on several key diagnostic tools:
- Imaging Tests:
- Chest X-rays to examine lungs and heart
- CT scans for detailed organ examination
- MRI scans for heart or nervous system involvement
- PET scans to detect inflammation
- Biopsy: Tissue confirmation through biopsy remains essential, especially if treatment is necessary. Depending on the affected organs, Doctors can obtain tissue samples through various methods. The most common approach is a bronchoscopy, which allows doctors to examine and take samples from the lungs and chest lymph nodes.
- Additional Diagnostic Procedures:
- Pulmonary function tests to measure lung capacity
- Blood tests to assess organ function
- Specialised eye examinations to detect eye-related problems
- Electrocardiogram (ECG) to monitor heart activity
Treatment for Sarcoidosis
Doctors typically adopt a "watch and wait" approach for mild cases, as the condition often resolves spontaneously.
When treatment becomes necessary, doctors focus on three primary goals: reducing inflammation, preventing organ damage, and improving quality of life.
The most commonly prescribed medications for sarcoidosis include:
- Corticosteroids: These powerful anti-inflammatory drugs serve as the first line of treatment
- Immunosuppressants: These antirejection medications help control the immune system's response
- Antimalarial Drugs: Hydroxychloroquine proves particularly effective for skin and joint symptoms
- TNF-alpha Inhibitors: These advanced medications target specific immune system chemicals
- Auxiliary Treatment: According to the symptoms or complications, doctors may prescribe additional treatments, including:
- Physical therapy to decrease fatigue and improve muscle strength
- Pulmonary rehabilitation to decrease respiratory symptoms
- Cardiac pacemaker or defibrillator for heart arrhythmias
When to See a Doctor
Recognising when to take advice from medical attention is crucial for managing sarcoidosis effectively. Patients should talk to their treating doctors immediately if they experience any new or worsening symptoms, particularly changes in breathing, vision problems, or irregular heartbeat.
Conclusion
Sarcoidosis remains a complex inflammatory condition that affects thousands of people worldwide. Medical science has made significant inroads in understanding and treating this disease, though its exact cause continues to puzzle researchers. Patients who receive early diagnosis and proper treatment often experience better outcomes and quality of life.
The journey with sarcoidosis looks different for each person. Some patients recover completely within a few years (2-3 years), while others need long-term medical care and monitoring. Regular check-ups, lifestyle modifications, and following prescribed treatment plans help patients manage their symptoms effectively.
FAQs
1. Who does sarcoidosis affect?
Sarcoidosis most commonly affects adults between ages 20 and 60. The condition shows higher prevalence in women and occurs more frequently in people of African and Northern European heritage. Healthcare workers, farmers, and firefighters face increased risk due to environmental exposures.
2. What are the stages of pulmonary sarcoidosis?
Pulmonary sarcoidosis is classified into five distinct stages:
- Stage 0: Normal chest X-ray with no visible signs
- Stage 1: Enlarged lymph nodes only
- Stage 2: Enlarged lymph nodes and lung involvement
- Stage 3: Lung involvement only
- Stage 4: Pulmonary fibrosis (permanent scarring)
3. How soon after treatment will I feel better?
Improvement occurs within a few weeks to months after starting treatment. The exact timeline varies depending on disease severity and individual response to medication. Regular monitoring helps doctors adjust treatment plans for optimal results.
4. What foods should be avoided with sarcoidosis?
Patients should limit refined foods, sugar, white pasta, and foods high in fat. Alcohol consumption should be minimised or avoided entirely, as it may interact with medications and affect liver function.
5. Is there a blood test for sarcoidosis?
Recent developments have led to promising blood tests for diagnosing sarcoidosis. While these tests show potential for faster diagnosis, they complement rather than replace traditional diagnostic methods like biopsies.
6. Is sarcoidosis a serious condition?
While most cases resolve within 2-3 years, sarcoidosis can be serious. About 10-20% of patients develop permanent organ damage. The condition requires careful monitoring and appropriate treatment to prevent complications.
7. What is the best diet for sarcoidosis?
A balanced, anti-inflammatory diet works best for managing sarcoidosis. This diet includes:
- Plenty of fruits, vegetables, and whole grains
- Lean proteins and healthy fats
- Foods rich in antioxidants & omega-3 fatty acids
To Book an Appointment, call:
Still Have a Question?




