-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Pulmonary Oedema
Symptom, Causes, Diagnosis and Treatment
Pulmonary Oedema
Fluid in the lungs affects millions of people worldwide and can become life-threatening without proper medical attention. This comprehensive blog explores the essential aspects of pulmonary oedema, from its early warning signs to various treatment approaches. Doctors use different strategies to manage this condition, including oxygen therapy, medications, and addressing the underlying cause.
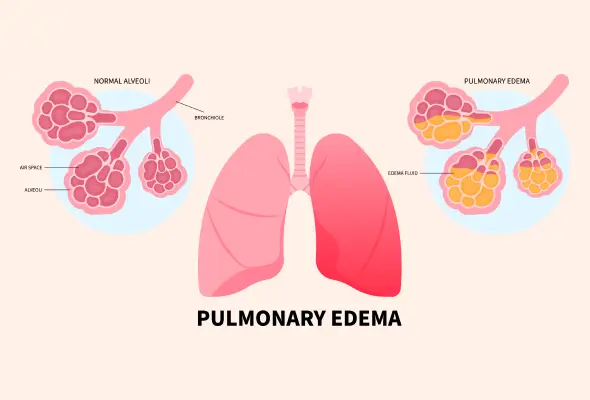
What is Pulmonary Oedema?
Pulmonary oedema is a serious medical condition characterised by an abnormal accumulation of fluid in the lungs' air sacs (alveoli). This fluid buildup interferes with normal breathing by preventing proper oxygen exchange in the lungs.
The following are common pulmonary oedema types:
- Cardiogenic Pulmonary Oedema: Occurs due to heart problems that affect the heart's ability to remove blood from the lungs effectively
- Non-cardiogenic Pulmonary Oedema: This oedema results from direct injury to the lung tissue. Various factors, including toxins, medications, or chest trauma, can cause.
When fluid collects in the lung's air sacs, it diminishes the crucial gas exchange process that usually occurs at the alveolar level. This disruption can progress to respiratory failure if left untreated. The severity of pulmonary oedema varies, with acute cases developing suddenly and requiring immediate medical intervention.
Pulmonary Oedema Symptoms
The symptoms of pulmonary oedema manifest differently depending on whether they develop suddenly or gradually over time.
- Sudden (Acute) Symptoms:
- Severe shortness of breath that worsens with activity
- A feeling of drowning or suffocating, especially when lying down
- Coughing up pink, frothy sputum
- Rapid, irregular heartbeat
- Wheezing or gasping for breath
- Cold, clammy skin
- Extreme anxiety or restlessness
- Long-term (Chronic) Symptoms:
- Breathlessness during physical activity
- Difficulty breathing when lying flat
- Waking up at night feeling short of breath
- New or worsening cough
- Swelling in legs and feet
- Unusual fatigue
- Rapid weight gain
Causes of Pulmonary Oedema
The condition develops through two distinct pathways, each with its own set of causes and risk factors.
- Cardiogenic Causes:
- Congestive heart failure
- Heart valve problems
- Coronary artery disease
- High blood pressure
- Irregular heart rhythms
- Cardiomyopathy (weakened heart muscle)
- Noncardiogenic Causes:
- Acute respiratory distress syndrome (ARDS)
- Severe infections or sepsis
- Exposure to toxins or smoke
- High-altitude exposure
- Near-drowning incidents
- Severe trauma or injury
Pulmonary Oedema Risk Factors
- Health Conditions: These include chronic kidney disease, liver problems, obstructive sleep apnoea, and severe infections.
- Environmental Factors: Individuals travelling to high-altitude locations above 8,000 feet may develop high-altitude pulmonary oedema, especially if they ascend too quickly without proper acclimatisation.
- Exposure to Certain Medications: Illegal drugs or toxic substances can damage the lungs and lead to fluid accumulation.
Complications of Pulmonary Oedema
As the condition advances, patients may experience several significant complications:
- Respiratory failure requiring mechanical ventilation
- Heart weakness and eventual heart failure
- Swelling in legs, feet, and abdominal area
- Fluid buildup around the lungs (pleural effusion)
- Liver congestion and swelling
- Acute Respiratory Distress Syndrome (ARDS)
Diagnosis
Diagnosing pulmonary oedema typically includes a thorough physical assessment and medical history review, mainly focusing on cardiovascular and lung conditions.
Doctors typically start with basic diagnostic tools:
- Blood Tests:
- BNP test to check for heart problems
- Complete blood count
- Kidney and thyroid function tests
- Electrolyte levels assessment
- Imaging Studies:
- Chest X-ray to confirm fluid in lungs
- CT scan for detailed lung examination
- Echocardiogram to assess heart function
- Lung ultrasound to detect fluid buildup
- Other Tests: Pulse oximetry and arterial blood gas tests help determine oxygen levels in the blood.
Treatment
- Oxygen Therapy: This therapy serves as the primary treatment for pulmonary oedema. Doctors deliver oxygen through various methods:
- Face mask or nasal cannula for mild cases
- Continuous positive airway pressure (CPAP) for moderate cases
- Mechanical ventilation for severe cases requiring breathing assistance
- Medications: Medications form an essential part of the treatment strategy. Doctors may prescribe several types of drugs to manage the condition effectively. These include diuretics to remove excess fluid, preload reducers to decrease heart and lung pressure, and afterload reducers to dilate blood vessels.
When to See a Doctor
Immediate medical intervention is necessary if someone experiences:
- Sudden and severe shortness of breath
- Chest pain or discomfort
- Pink or bloody frothy sputum when coughing
- Blue or grey tinting of lips or nails
- Confusion or drowsiness
- Rapid heartbeat with sweating
- Severe anxiety or feeling of suffocation
- Difficulty breathing when lying flat
- Persistent cough lasting more than 2-3 weeks
Prevention
Doctors recommend specific lifestyle modifications and preventive measures to lower the possibility of developing this serious pulmonary condition.
Essential Prevention Strategies:
- Control blood pressure through regular monitoring and medication adherence
- Maintain proper management of existing heart and lung conditions
- Follow a balanced diet low in salt (less than 2,300 mg daily)
- Exercise regularly with at least 120-150 minutes of moderate activity weekly
- Keep a healthy weight through proper nutrition
- Avoid smoking and exposure to secondhand smoke
- Get routine vaccinations to prevent respiratory infections
For individuals planning high-altitude activities, specific precautions help prevent high-altitude pulmonary oedema:
- Gradual ascent, increasing elevation by no more than 1,000 feet per day above 8,200 feet, helps.
- Taking preventive medications like acetazolamide or nifedipine
Conclusion
The outlook for pulmonary oedema patients continues to improve as medical knowledge expands. People who follow their treatment plans and make recommended lifestyle changes often see significant improvements in their quality of life. Success in managing pulmonary oedema depends on both medical intervention and patient commitment to following prevention strategies.
FAQS
1. What's the difference between pulmonary oedema and pneumonia?
While both conditions affect the lungs, they have distinct characteristics. Pulmonary oedema involves fluid accumulation in the air sacs, while pneumonia is an infection causing inflammation in the lungs. Pneumonia typically causes fever and productive cough with thick mucus, whereas pulmonary oedema often produces pink, frothy sputum.
2. What is the leading cause of pulmonary oedema?
Heart problems, particularly congestive heart failure, represent the most common cause of pulmonary oedema. The condition develops when the heart cannot effectively pump blood, resulting in increased pressure in the lung's blood vessels and subsequent fluid leakage into the air sacs.
3. How do you tell if you have fluid in your lungs?
Doctors identify fluid in the lungs through several indicators:
- Crackling sounds when listening to the lungs
- Rapid breathing and increased heart rate
- Swelling around the neck and abdomen
- Pale or bluish skin tone
4. How do you remove fluid from the lungs?
Doctors use various methods to remove excess fluid, including:
- Diuretic medications to increase fluid removal
- Supplemental oxygen therapy
- Thoracentesis procedure for severe cases
- Treatment of underlying heart conditions
5. Can lungs clear themselves of fluid?
The lungs naturally clear small amounts of fluid through their drainage system. However, in pulmonary oedema, the fluid accumulation exceeds the lungs' natural clearing capacity, requiring medical intervention.
6. Can a person recover from pulmonary oedema?
Most people can recover from pulmonary oedema with proper treatment. The recovery timeline varies and depends on the underlying cause and treatment adherence. Moderate cases often show improvement within 6 months to a year with appropriate medical care and lifestyle modifications.
Still Have a Question?




