-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Pleural Effusion
Symptom, Causes, Diagnosis and Treatment
Pleural Effusion
Pleural effusion condition affects millions of people globally each year. The causes vary widely, from heart failure and infections to cancer and inflammatory conditions. This article explores the reasons, symptoms, and treatment options available for managing pleural effusion effectively.
What is Pleural Effusion?
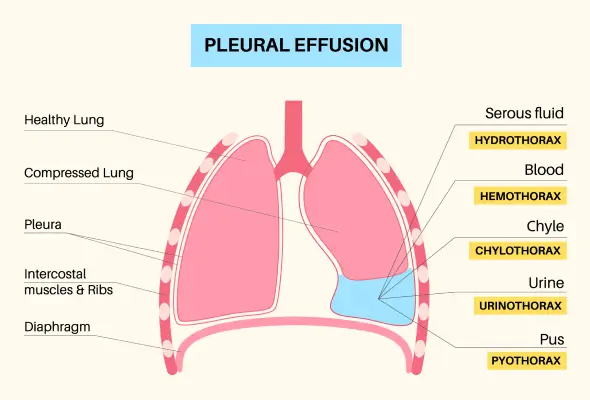
The pleural space contains a thin layer of fluid between two membranes surrounding the lungs. Fluid in the lungs (pleural effusion) develops when excess fluid accumulates in this space, disrupting the normal balance between fluid production and absorption. Doctors classify pleural effusions into two main types:
- Transudative Effusions: These occur when fluid is pushed through blood vessel walls due to pressure changes, often seen in heart failure
- Exudative Effusions: These develop when inflammation causes fluid to leak from blood vessels, commonly associated with infections or cancer
The pleural membranes continuously produce and absorb fluid to maintain proper lung function. When this balance is disrupted, either through increased fluid production or decreased absorption, pleural effusion develops. This excess fluid can compress the lungs, making it harder for them to expand fully during breathing.
Pleural Effusion Symptoms
Patients with pleural effusion may experience varying degrees of symptoms depending on the amount of fluid accumulated in the pleural space. Some individuals might not notice any symptoms, mainly when the fluid buildup is minimal.
When symptoms do occur, they typically include:
- Shortness of breath (dyspnoea), which often worsens with physical activity
- Chest pain, particularly noticeable during deep breathing
- A persistent cough that may be dry or productive
- Fever, especially if the underlying cause is an infection
- Difficulty breathing when lying flat (orthopnea)
- General discomfort in the chest area
Causes and Risk Factors of Pleural Effusion
Doctors classify the causes of pleural effusion based on the type of fluid that accumulates in the pleural space. Understanding these causes helps determine the most effective treatment approach.
The following are two main categories of pleural effusion causes:
- Transudative Causes
- Heart failure
- Liver cirrhosis
- Kidney disorders (nephrotic syndrome)
- Fluid imbalance conditions
- Exudative Causes
- Lung infections (pneumonia, tuberculosis)
- Cancer (especially lung and breast cancer)
- Inflammatory conditions
- Post-cardiac surgery complications
- Autoimmune diseases
Several risk factors can elevate a person's likelihood of developing pleural effusion. These are:
- Age: Certain types are more common in people aged 15-34 and those over 55 Medical History: Heart conditions, kidney disease, and autoimmune disorders
- Lifestyle Choices: Smoking tobacco contributes to the development of pleural disorders
- Medication Reactions: Reactions to drugs like methotrexate and amiodarone.
- Chest Injuries: It can lead to fluid accumulation in the pleural space.
Complications of Pleural Effusion
The most severe complications include:
- Empyema: An infection that develops when bacteria invade the pleural space, leading to pus accumulation and potential sepsis
- Pleural Thickening: Formation of fibrous tissue that restricts lung expansion and breathing
- Lung Damage: Chronic compression of lung tissue from fluid buildup can cause permanent damage
- Respiratory Compromise: Decreased lung function due to restricted expansion
- Abscess Formation: Development of infected pockets within the pleural space
Treatment procedures themselves can sometimes lead to additional complications. Patients undergoing treatment may experience pulmonary oedema, blood clots, or abnormal heart rhythms. In some cases, procedures like thoracentesis might result in a pneumothorax (collapsed lung), though this is relatively rare when performed by experienced doctors.
Diagnosis
When patients present with symptoms or when routine chest imaging reveals fluid accumulation, experts advise several imaging techniques to confirm the presence of pleural effusion:
- Chest X-rays: Often the first test to detect fluid buildup
- Ultrasound: Helps visualise small effusions and guide fluid removal
- CT Scans: Provides detailed images and can reveal underlying causes
- MRI: Sometimes used for complex cases or to evaluate questionable findings
- PET Scans: Doctors may also use specialised imaging techniques like PET scans to identify specific causes, particularly when cancer is suspected.
- Thoracentesis: Once imaging confirms the presence of fluid, doctors perform a diagnostic procedure- thoracentesis to collect a fluid sample. This involves inserting a needle into the pleural space to extract fluid for further analysis. The fluid undergoes various tests to determine whether it is transudative or exudative, which helps identify the underlying cause.
- Laboratory analysis of the pleural fluid may include tests for protein levels, LDH (lactate dehydrogenase), cell counts, and cultures for infection.
Treatment
The following are some common pleural effusion treatment approaches:
- Medication Management:
- Diuretics for heart-related effusions
- Antibiotics for infectious causes
- Chemotherapy for malignant cases
- Fluid Drainage Procedures:
- Therapeutic thoracentesis for symptom relief
- Chest tube placement for continuous drainage
- Small-bore drains (10-14 gauge) for patient comfort
Doctors carefully monitor fluid removal, limiting extraction to 1,500 ml per session to prevent complications like pulmonary oedema or collapsed lung.
- Procedures: For recurring effusions, doctors may recommend more permanent solutions. Pleurodesis, a medical procedure that creates controlled scarring to prevent fluid buildup, offers about 50% success in preventing future effusions. Some patients benefit from tunnelled catheter placement, allowing them to drain fluid at home as needed.
- Surgery: Surgical interventions become necessary when other treatments prove ineffective. Video-assisted thoracoscopic surgery (VATS) uses small incisions to manage difficult cases, while traditional thoracotomy may be required for severe infections.
When to See a Doctor
Individuals should immediately seek medical care if they experience:
- Severe breathing difficulties or shortness of breath
- Sharp chest pain that worsens with breathing
- Sudden onset of breathing problems
- Blue tinge to lips or skin
- Rapid breathing with chest tightness
Prevention
Taking proactive steps to prevent pleural effusion involves both lifestyle modifications and regular medical monitoring. Doctors recommend these preventive measures:
- Regular Physical Activity: Engaging in appropriate exercise routines helps maintain overall lung health
- Healthy Diet: Following a balanced, low-salt diet, particularly for those with heart conditions
- Smoking Cessation: Avoiding tobacco products reduces respiratory risks
- Occupational Safety: Using proper respiratory protection in hazardous work environments
- Vaccination: Getting immunised against pneumonia and influenza
- Regular Check-ups: Scheduling routine medical examinations, especially for those with underlying conditions
Conclusion
Prevention strategies, including regular exercise, proper diet, and routine medical check-ups, help reduce the risk of developing pleural effusion. People with existing health conditions should work closely with their doctors to manage their conditions and prevent complications. Patients can effectively manage pleural effusion and maintain their quality of life through proper medical care and lifestyle modifications.
FAQS
1. What is the difference between pleural effusion and pericardial effusion?
While both conditions involve fluid accumulation, they affect different chest areas. Pleural effusion occurs in the space around the lungs, while pericardial effusion develops in the sac surrounding the heart. This difference in location leads to distinct symptoms and requires different treatment approaches.
2. What is the leading cause of pleural effusion?
Congestive heart failure stands as the most common cause of pleural effusion. Other significant causes include:
- Infections like pneumonia and tuberculosis
- Cancer (particularly lung and breast cancer)
- Liver or kidney disease
3. How to remove pleural effusion?
Doctors typically remove pleural effusion through a procedure called thoracentesis, where they insert a needle between the ribs to drain the fluid. For recurring cases, doctors might recommend:
- Chest tube placement
- Long-term catheter insertion
- Surgical interventions in severe cases
4. How much pleural fluid is normal?
A healthy person typically has about 10-20 millilitres of pleural fluid, equivalent to a few teaspoons. This small amount helps lubricate the space between the lungs and chest wall during breathing.
5. How long does it take to recover from a pleural effusion?
Recovery time varies based on the underlying cause and treatment method. Most patients recover within 2-4 weeks after treatment, though some may require longer recuperation periods, especially after surgical interventions.
6. Is pleural effusion painful?
Many patients experience chest pain, particularly during deep breathing or coughing. The pain typically feels sharp and may worsen with movement or lying down.
7. Can pleural effusion go away naturally?
Minor pleural effusions may resolve naturally, mainly if caused by viral infections. However, most cases require medical intervention to treat the underlying condition and prevent complications.
Still Have a Question?




