-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Plantar Fasciitis
Symptom, Causes, Diagnosis and Treatment
Plantar Fasciitis
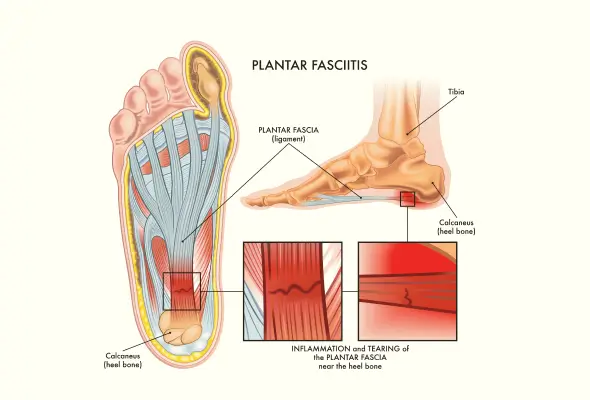
Plantar fasciitis arises when the plantar fascia, a strong, fibrous band of tissue running from the heel to the ball of the foot, becomes inflamed. This condition stands as the most prevalent cause of heel pain, affecting millions of individuals annually.
The plantar fascia functions as a crucial component in foot mechanics, resembling a thick rubber band in its elasticity. This remarkable tissue connects the foot bones, forming the arch underneath while providing essential shock absorption during movement. The fascia comprises three distinct segments originating from the calcaneus (heel bone), working together to maintain normal foot biomechanics.
Despite its name suggesting inflammation (-itis suffix), plantar fasciitis involves degenerative irritation at the plantar fascia's origin point, specifically at the medial calcaneal tuberosity of the heel and surrounding perifascial structures.
Plantar Fasciitis Symptoms
Pain stands as the primary indicator of plantar fasciitis, manifesting in distinct patterns throughout the day. The most intense discomfort typically strikes upon taking the first steps after waking up in the morning. Furthermore, this characteristic morning pain, often called "first-step pain," generally subsides within 5 to 10 minutes of movement.
The pain associated with plantar fasciitis presents itself in various forms:
- A dull, constant ache in the affected foot
- Sharp or stabbing sensations, particularly when applying pressure
- Increased discomfort after periods of inactivity
- Pain that temporarily improves with exercise but worsens afterwards
The location of discomfort primarily centres around the heel area, extending along the bottom of the foot. Individuals might experience heightened pain intensity under certain circumstances, such as walking barefoot or wearing shoes with minimal support.
Beyond pain, several additional symptoms accompany plantar fasciitis.
- The affected area often exhibits stiffness, particularly in the heel region.
- Many individuals notice swelling around their heel and tightness in the Achilles tendon.
- For some individuals, the pain develops gradually over time; however, the onset can be sudden in some instances, particularly following incidents such as missing a step or landing forcefully from a height.
- After periods of rest or sitting, standing up often triggers increased discomfort. Physical activity presents an interesting paradox - moderate movement might temporarily alleviate the pain, but prolonged or vigorous activity frequently exacerbates symptoms.
Plantar Fasciitis Causes
Several factors can contribute to the development of plantar fasciitis. Medical research points to three primary risk factors:
- Reduced ankle flexibility
- Excess body weight
- Prolonged standing
The condition often stems from repetitive strain, causing micro-tears in the plantar fascia. Common contributing factors include:
- Foot Structure Issues:
- High arch feet
- Flat feet
- Excessive pronation or supination
- Activity-related Factors:
- Sports participation
- Exercise without a proper warm-up
- Working on hard surfaces
- A sudden increase in activity levels
- Footwear Choices:
- Inadequate foot support
- Regular use of flip-flops
- Walking barefoot frequently
- Biomechanical Factors:
- Tightness in the gastrocnemius and soleus muscles
- Pes planus increases tension at the plantar fascia's origin
- Pes cavus reduces the foot's natural shock absorption capacity.
Complications of Plantar Fasciitis
Untreated plantar fasciitis leads to various complications that affect daily life.
Small tears accumulate gradually, weakening the ligament's strength and stability. Subsequently, these tears multiply in size and number, making the plantar fascia increasingly vulnerable to rupture.
A plantar rupture represents a severe complication, marked by a distinct popping sound accompanied by intense pain, bruising, and swelling in the foot.
Heel spurs develop as another significant complication. The body responds to untreated plantar fasciitis by depositing calcium near the foot's arch. These calcium deposits form sharp protrusions that press against the heel's fatty tissue, resulting in heightened pain with each step.
Plantar fibromatosis is a distinct complication characterised by benign nodules growing along the plantar fascia.
Long-term complications extend beyond the foot, affecting overall mobility. Untreated plantar fasciitis alters walking patterns as individuals unconsciously adjust their gait to minimise pain. This compensation leads to:
- Pain throughout the kinetic chain
- Ankle discomfort
- Knee problems
- Hip complications
- Lower back issues
Diagnosis of Plantar Fasciitis
Doctors examine the foot by applying gentle pressure to identify tender areas. The most telling sign emerges upon pressing the medial plantar calcaneal region, often triggering a sharp, stabbing sensation. Throughout the examination, doctors observe walking patterns, as individuals might unconsciously adopt an equine position to avoid heel pressure.
The diagnostic process involves several key tests:
- Windlass Test: Doctors perform passive dorsiflexion of the first metatarsophalangeal joint. A positive result occurs if this movement reproduces pain at the plantar fascia.
- Ankle Flexibility Assessment: Doctors check for limited ankle dorsiflexion, often linked to a tight Achilles tendon.
- Foot Structure Evaluation: Examination includes checking for flat feet, high arches, or leg length differences that might contribute to the condition.
Plantar Fasciitis Treatment
Conservative treatments form the cornerstone of plantar fasciitis management.
- Icing the affected area for 10-15 minutes twice daily helps reduce inflammation.
- A frozen water bottle wrapped in a thin towel serves as an effective tool for ice massage along the foot's bottom.
- Rest proves essential in the healing process. Taking breaks from activities that worsen symptoms allows the plantar fascia to recover.
- Over-the-counter NSAIDs effectively manage pain and inflammation.
- Physical therapy stands as a crucial component of treatment.
- Stretch the plantar fascia and Achilles tendon
- Strengthen lower leg muscles
- Apply athletic taping techniques
- Teach proper massage methods
- Supportive footwear plays a vital role in recovery. Night splints offer an effective solution by maintaining the plantar fascia & Achilles tendon in a lengthened position overnight.
- For persistent cases, doctors might recommend:
- Corticosteroid injections for temporary pain relief
- Platelet-rich plasma treatment to promote tissue healing
- Extracorporeal shock wave therapy shows promising results in reducing heel pain
- Surgery remains a rare necessity, reserved exclusively for severe cases unresponsive to other treatments.
When to See a Doctor
Certain warning signs necessitate immediate medical consultation:
- Pain extending beyond the heel area
- Consistent increase in discomfort after rest periods
- Constant, unrelenting foot pain
Conclusion
Plantar fasciitis remains a highly treatable condition when addressed early. Most patients achieve full recovery through simple conservative treatments like rest, ice, and proper footwear. While the healing process requires patience, dedicated adherence to treatment plans leads to positive outcomes.
Above all, prevention plays a key role in managing plantar fasciitis. Simple lifestyle alterations such as maintaining a healthy weight, wearing supportive shoes, and proper exercise warm-up routines help reduce the risk of developing this condition. Regular foot stretches and exercises strengthen the plantar fascia, making it more resilient to daily stress.
FAQs
1. Is plantar fasciitis serious?
Plantar fasciitis rarely requires surgical intervention. Most patients recover completely within 6-18 months through non-surgical approaches.
2. What is the leading cause of plantar fasciitis?
Overuse stands as the primary trigger for plantar fasciitis. Certain activities increase the risk substantially:
- Standing all day at work
- Having a BMI over 30 kg/m²
- Limited ankle flexibility
3. What is the fastest cure for plantar fasciitis?
Quick relief involves multiple approaches working together:
- Rest and ice therapy
- Daily stretching exercises
- Supportive footwear
- Arch-supporting inserts
- Anti-inflammatory medication
- Physical therapy sessions
4. What foods should I avoid with plantar fasciitis?
Diet influences inflammation levels in plantar fasciitis. Foods to avoid include:
- Highly processed items
- Refined carbohydrates (white bread, pasta)
- Fried foods
- High-fat dairy products
- Red meat
- Sweetened beverages
- Trans fats (margarine, shortening)
5. What is the best natural remedy for plantar fasciitis pain?
Natural remedies offer effective relief options:
- Lavender essential oil massage (diluted with carrier oil)
- Regular foot stretches
- Golf ball rolling exercises
- Ice pack applications (15-20 minutes, 3-4 times daily)
- Weight management through balanced nutrition
Still Have a Question?


