-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Pericarditis
Symptom, Causes, Diagnosis and Treatment
Pericarditis
A common heart problem, pericarditis affects the protective sac around your heart, causing discomfort and concern for many. Pericarditis occurs when this sac, called the pericardium, becomes inflamed. It can happen to anyone at any age and impacts overall heart health. Understanding pericarditis is crucial to recognising its symptoms and getting the proper treatment.
This article delves into the world of pericarditis to give you a clear picture. We'll explore the different types of pericarditis, what causes it, and the signs to watch out for. You'll learn about the risk factors, possible complications, and how doctors diagnose this condition.
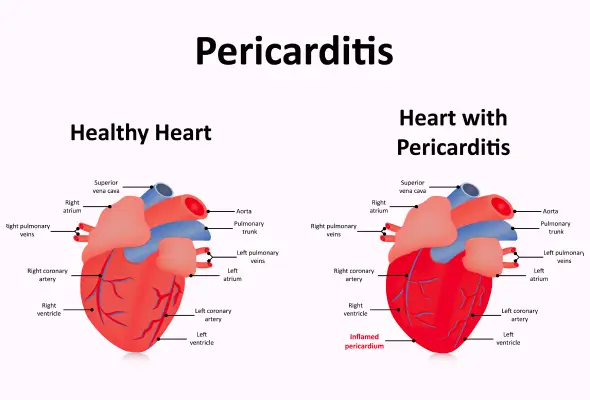
What is Pericarditis?
Pericarditis is an inflammation of the pericardium, a thin, two-layered, fluid-filled sac that covers the heart's outer surface. This protective membrane provides lubrication, shields the heart from infection, and keeps it from overexpanding. When pericarditis occurs, the pericardium becomes red and swollen, similar to inflamed skin around a cut. This heart problem can affect anyone but is most common in men aged 16 to 65. Pericarditis usually develops suddenly and may last for weeks or months. It can sometimes lead to pericardial effusion, where extra fluid accumulates between the pericardial layers.
Pericarditis Types
Pericarditis has several types based on its duration and causes:
- Acute pericarditis develops suddenly, with symptoms lasting less than four to six weeks.
- Incessant pericarditis persists for four to six weeks but less than three months despite treatment.
- Chronic pericarditis lasts more than three months.
- Recurrent pericarditis occurs when symptoms return after a symptom-free period of at least four weeks.
- Infectious pericarditis caused by viruses, bacteria, or fungi.
- Idiopathic pericarditis with no apparent known cause.
- Traumatic pericarditis results from chest injuries.
- Uremic pericarditis develops due to kidney failure.
- Malignant pericarditis is associated with cancer.
Understanding these types helps appropriately diagnose and manage this heart problem.
Pericarditis Causes
Pericarditis has various causes, both infectious and non-infectious.
- Infectious Pericarditis:
- Viruses are the most common culprits, including coxsackieviruses, echovirus, and adenoviruses.
- Though less frequent in developed countries, bacterial infections can also lead to pericarditis.
- Tuberculosis is prevalent in developing nations, especially among HIV-positive individuals.
- In rare cases, fungi like Histoplasma or parasites such as Toxoplasma can cause pericarditis, particularly in people with weakened immune systems.
- Non-infectious Pericarditis:
- Autoimmune diseases like lupus and rheumatoid arthritis.
- Metabolic conditions such as kidney failure.
- Trauma, either from injury or medical procedures, can also trigger pericarditis.
- Some medications, including certain cancer treatments, may cause this heart problem.
- Idiopathic Pericarditis:
- In up to 90% of cases, the cause remains unknown, resulting in a diagnosis of idiopathic pericarditis.
Pericarditis Symptoms You Should Be Aware Of
- Pericarditis often causes sharp, stabbing chest pain that comes on suddenly. This discomfort typically occurs in the middle or left side of the chest and may extend to one or both shoulders.
- The pain worsens when lying down or breathing deeply, but sitting up and leaning forward can provide relief.
- Individuals may experience fever, weakness, and trouble breathing.
- Some people experience palpitations, feeling their heart skipping beats or beating irregularly.
- In chronic cases, tiredness and shortness of breath are common.
- Severe pericarditis can lead to swelling in the stomach, feet, and legs, along with low blood pressure.
- If you have any of these signs or symptoms of pericarditis, especially chest pain, seek medical attention immediately.
Risk Factors
Pericarditis can affect anyone, but certain factors increase the risk, such as:
- Men between 16 and 65 years old are more likely to develop this heart problem.
- People who have had a heart attack, open heart surgery, or radiation therapy are at higher risk.
- Autoimmune diseases, kidney failure, and HIV/AIDS also raise the chances of pericarditis.
- Those with a history of rheumatic fever or hypothyroidism face increased risk.
- Certain medications like phenytoin and heparin may trigger pericarditis in rare cases.
- Individuals who experience frequent dry coughs, abnormal body temperatures, or have broken blood vessels in their lungs and eyes are more susceptible.
- About 15% to 30% of those treated for acute pericarditis may have recurrences if not given proper medication.
Complications of Pericarditis
Pericarditis can lead to serious complications if left untreated, such as:
- Cardiac tamponade (fluid builds up rapidly in the pericardium, compressing the heart)
- Constrictive pericarditis
- Chronic effusive pericarditis
Pericarditis Diagnosis
Diagnosing pericarditis involves a combination of methods.
- Medical History and Auscultation: Doctors typically examine patients and ask about their symptoms and medical history. They listen to the heart using a stethoscope, checking for a distinctive sound called a pericardial rub. This noise occurs when the inflamed layers of the pericardium rub against each other.
- Blood Tests: Different blood tests help check for signs of inflammation, infection, or heart attack.
- Electrocardiogram: An ECG records the heart's electrical signals, showing characteristic changes in pericarditis. Pericarditis on ECG shows diffuse ST-segment elevation and PR-segment depression.
- Chest X-rays: A chest X-ray can reveal an enlarged heart
- Echocardiogram: This ultrasound creates images of the heart, detecting fluid buildup or pumping issues.
In some cases, doctors may conduct advanced imaging like CT scans or MRIs to confirm the diagnosis and rule out other conditions.
Treatment for Pericarditis
The choice of pericarditis treatment depends on its severity and underlying cause:
- Wait and Watch: Mild cases may improve without intervention, while more serious ones require medical attention.
- Pericarditis Medication: Doctors may prescribe pain relievers to manage discomfort and reduce inflammation. Colchicine, an anti-inflammatory medication, may treat acute pericarditis or prevent recurrences.
- In some cases, corticosteroids or immunosuppressants are necessary to control persistent inflammation.
- If a bacterial infection is the cause, doctors may administer antibiotics.
- Surgical Intervention: For fluid buildup around the heart, doctors perform procedures such as pericardiocentesis to drain the excess fluid. In severe cases of constrictive pericarditis, surgical removal of part or all of the pericardium might be required.
When to See a Doctor
- If you experience new symptoms of chest pain, it's crucial to seek medical care immediately.
- Many pericarditis symptoms resemble those of other heart and lung conditions, so getting a thorough check-up from a healthcare professional is essential. This is particularly important if you have a history of acute pericarditis and notice returning symptoms or changes in your condition during recovery.
- Watch out for chest pain, fever, and trouble breathing.
Prompt medical intervention is vital for proper diagnosis and treatment of pericarditis or any other potential heart problems.
Preventions
While preventing pericarditis isn't always possible, there are steps to lower the risk of the condition, such as:
- Protect the chest area during activities to prevent injury-related pericarditis.
- Managing chronic systemic conditions, such as autoimmune diseases (like lupus or rheumatoid arthritis), kidney disease, or cancer, is crucial.
- A heart-healthy diet, avoiding coffee and alcohol, quitting smoking, and stress reduction techniques like meditation can help.
- Follow-up care after heart surgery or a heart attack is essential, as these can increase the risk of developing pericarditis. Rest, moderate physical activity, and a healthy diet significantly prevent complications.
Conclusion
Pericarditis is a heart condition that affects many people's lives. By recognising the signs of pericarditis and its risk factors, individuals can seek timely medical attention, which is vital for appropriate diagnosis and treatment. The various diagnostic methods and treatment options discussed offer hope for those affected by this condition.
Understanding pericarditis empowers patients and their loved ones to take an active part in managing the condition. While prevention isn't always possible, adopting a heart-healthy lifestyle and following medical advice can help reduce the risk of recurrence. Remember, if you experience chest pain or other symptoms, see a doctor promptly. With proper care and management, many people with pericarditis can lead full and active lives.
FAQ's
1. What is the difference between myocarditis and pericarditis?
Myocarditis affects the heart muscle, while pericarditis involves inflammation of the pericardium, the protective sac surrounding the heart. Both conditions can cause chest pain, but pericarditis pain often improves when sitting up and leaning forward. Myocarditis typically causes fatigue and shortness of breath. Both can result from viral infections, but pericarditis is more common and generally has a better prognosis.
2. Who does pericarditis affect?
Pericarditis can affect anyone, but it's most common in men aged 16 to 65. Individuals with a history of heart attacks, open heart surgery, or radiation therapy are at higher risk. Those with autoimmune diseases, kidney failure, or HIV/AIDS also face an increased chance of developing pericarditis.
3. How does pericarditis affect my body?
Pericarditis causes inflammation of the pericardium, making it red and swollen. This can lead to chest pain, especially when breathing deeply or lying down. In some cases, fluid can accumulate between the pericardial layers, potentially affecting the heart's ability to pump effectively.
4. How serious is pericarditis?
While pericarditis is often mild and self-limiting, it can be serious in some cases. Complications may include cardiac tamponade, where fluid buildup around the heart impairs its function, or constrictive pericarditis, where the pericardium becomes thick and stiff. These complications can be fatal if not addressed promptly. However, with proper treatment, most people with pericarditis recover fully.
5. Will pericarditis go away on its own?
Mild cases of pericarditis may resolve without treatment. However, most cases require medical intervention to manage symptoms and prevent complications. Treatment typically involves anti-inflammatory medications and rest. The condition usually clears up within three months, but in some cases, it can become chronic or recurrent. Up to 30% of patients may experience recurrence within 18 months of the initial episode.
6. Is walking ok with pericarditis?
During active pericarditis, it's crucial to avoid strenuous activity. Light walking may be acceptable but always consult your doctor first. As you recover from pericarditis, your doctor will advise you to increase your physical activity gradually. For competitive athletes, a minimum restriction of three months is often recommended, followed by a routine workup to exclude active disease before returning to sports.
7. What foods are bad for pericarditis?
While there's no specific diet for pericarditis, certain foods may exacerbate inflammation. It's advisable to avoid fried, greasy, and spicy meals, processed meats, and high-salt foods. Limiting alcohol, caffeine, and high-sugar foods is also recommended. A heart-healthy diet with minimally processed foods is generally beneficial. Always consult your doctor for personalised dietary advice.
Still Have a Question?