-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Osteosarcoma
Symptom, Causes, Diagnosis and Treatment
Osteosarcoma
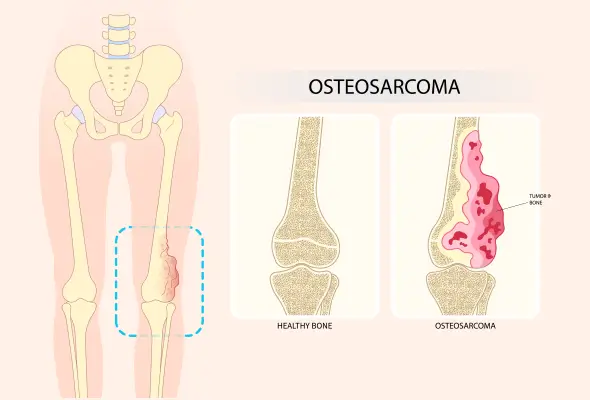
Osteosarcoma bone cancer is a rare but serious form of cancer that starts in the cells that make bone. This type of cancer most often affects children, teenagers, and young adults, causing pain and swelling in the affected area. Understanding osteosarcoma cancer symptoms and treatment options is crucial for early detection and effective management. This article explores the causes of osteosarcoma, its various types, and common osteosarcoma symptoms to watch for.
What is Osteosarcoma?
Osteosarcoma cancer, or osteogenic sarcoma, is the most prevalent cancer of the bone, and it starts in the cells responsible for making new bone. This rare form of cancer typically develops in the osteoblast cells, which are crucial for bone formation. However, the bone produced by these cancerous cells is not as strong as normal bone.
Osteosarcoma bone cancer most often affects long bones, such as those in the arms and legs. It usually occurs near the ends of these bones, known as the metaphyses, particularly around the knee, where rapid growth occurs in teenagers. The most common locations for osteosarcoma include the femur (thigh bone) near the knee, the tibia (shin bone) near the knee, and the humerus (upper arm bone) near the shoulder.
While osteosarcoma can develop in any bone in the body, it is less common in areas such as the pelvis, skull, and jaw. In rare cases, it may even affect soft tissues or organs in the abdomen or chest.
This type of cancer has a tendency to grow into nearby healthy tissues, such as tendons or muscles. It can also spread or metastasise through the bloodstream to other organs or bones in the body.
Types of Osteosarcoma
Osteosarcoma bone cancer can be classified into several types, each with its own characteristics and locations within the body. The two main categories are:
- Primary Osteosarcomas: These occur due to abnormalities in bone development and are more common in children and teenagers whose bones are still growing. These are further divided into three main types:
- Intramedullary Osteosarcoma: This osteosarcoma is the most common type, accounting for about 80% of all osteosarcoma diagnoses. It develops in the medullary cavity of long bones, such as the femur. Subtypes include osteoblastic, chondroblastic, fibroblastic, small-cell, and epithelioid.
- Juxtacortical Osteosarcoma: This type makes up 10-15% of all diagnoses and develops on the outer surface of bones or the periosteum, the dense layer of connective tissue covering the bones.
- Extraskeletal Osteosarcoma: This rare type accounts for less than 5% of all diagnoses. These tumours arise in soft tissues and are not attached to bone, often occurring at sites of previous radiation therapy.
- Secondary Osteosarcomas: These typically occur in adults with fully formed bones and are usually considered higher-grade malignancies than primary osteosarcomas.
- Other rare subtypes include parosteal, periosteal, telangiectatic, and small-cell osteosarcoma.
Causes And Risk Factors of Osteosarcoma
The exact cause of osteosarcoma bone cancer remains unknown. However, researchers believe it results from a complex interplay of genetic and environmental factors. While the precise development mechanisms are not fully understood, several risk factors have been recognised that may increase the likelihood of developing this rare form of cancer. These are:
- Age: The condition predominantly affects children, teenagers, and young adults, with the highest risk occurring between 10 and 30. This suggests a possible link between rapid bone growth during puberty and the development of osteosarcoma.
- Gender: Interestingly, females tend to develop the condition slightly earlier than males, possibly due to earlier growth spurts.
- Genetic Factors: Certain inherited cancer syndromes, such as Li-Fraumeni syndrome, hereditary retinoblastoma, and Rothmund-Thomson syndrome, are associated with an increased possibility of developing osteosarcoma. These syndromes are due to specific genetic mutations, including TP53, RB1, and REQL4, respectively.
- Previous Exposure to Radiation Therapy: RT, particularly at a young age or with high doses, can increase the risk of osteosarcoma.
- Bone Diseases: Paget's disease and fibrous dysplasia have been linked to a higher risk of osteosarcoma.
Symptoms of Osteosarcoma
Osteosarcoma bone cancer often presents with a range of symptoms that can vary in intensity and progression, including:
- Bone Pain: The most common sign is persistent bone pain that worsens over time, particularly at night.
- Swelling and Redness: Pain may be accompanied by swelling and redness at the site of the tumour.
- Lump: As the condition progresses, individuals may notice a lump or mass over the bone, which can feel warm.
- Fracture: Sometimes, the weakened bone may fracture more easily than normal, even with simple movements.
- Other symptoms may include:
- Unexplained fever
- Exhaustion
- Anaemia
- Unexplained weight loss
- Limited movement, particularly if a joint is affected
Complications
Osteosarcoma bone cancer can lead to various complications, both from the disease itself and osteosarcoma treatment. These include:
- Metastasis: It is the spread of cancer to other parts of the body. Osteosarcoma most commonly spreads to the lungs, the same or another bone.
- Treatment-related Complication:
- Chemotherapy may lead to nausea, fatigue, hair loss, anaemia, and loss of appetite in the short term. Long-term adverse effects can include heart and lung damage, gradual hearing loss, and an increased risk of other cancers.
- Radiation therapy can cause similar long-term effects, as well as fertility issues if directed at the pelvic area.
- Additionally, wound infections and slow healing may occur after surgery.
- Problems with bone grafts or prostheses, such as infection or implant failure, can also arise.
Diagnosis
- Physical Examination: Doctors will assess the affected area for swelling, lumps, or movement difficulties.
- Imaging Tests:
- X-rays: Diagnostic X-rays are the initial imaging method and can effectively detect bone abnormalities caused by cancer.
- MRI Scans: They provide detailed images of bones and soft tissues
- CT Scans: They are beneficial for checking if the cancer has spread to the lungs.
- Bone Scan: They may also be performed to gather more information about the inside of the bones.
- Biopsy: It is the most definitive way to diagnose osteosarcoma and involves taking a sample of affected bone tissue for laboratory analysis.
Treatments
The treatment of osteosarcoma bone cancer typically involves a combination of surgery and chemotherapy. The approach depends on the stage and location of the bone sarcoma, as well as the patient's overall health.
- Surgery: The main goal is to remove all the cancer cells while preserving as much function and appearance as possible.
- Limb-sparing Surgery: Here, the tumour and some surrounding healthy tissue are removed.
- Amputation: It may be necessary if the cancer has spread extensively or if limb-sparing surgery is not feasible.
- Chemotherapy: It's usually given before surgery (neoadjuvant chemotherapy) to shrink the tumour mass and make it easier to remove. After surgery, more chemotherapy (adjuvant chemotherapy) is given to kill any remaining cancer cells and decrease the risk of recurrence.
- Radiation Therapy: It might be an option if surgery isn't possible or if all the cancer can't be removed during surgery.
When to See a Doctor
If you or your child experiences persistent bone pain that lasts for several weeks, it's crucial to schedule an appointment with a doctor promptly. While these symptoms can be caused by many things other than osteosarcoma bone cancer, such as sports injuries, any ongoing bone discomfort should be checked by a doctor.
Conclusion
Osteosarcoma bone cancer is a serious condition that needs quick action and good care. While it's not a common condition, it can significantly impact those who get it, especially young people. Getting help early is key to dealing with osteosarcoma. If you or someone you know has ongoing bone pain or swelling, immediately consult a doctor. With the proper care and support, many people with osteosarcoma can get better and live full lives.
FAQs
1. Who is at risk for developing osteosarcoma?
Osteosarcoma bone cancer primarily affects children, teenagers, and young adults with a slightly higher risk in people with certain genetic conditions, such as Li-Fraumeni syndrome or hereditary retinoblastoma or those who have undergone radiation therapy or have specific bone diseases like Paget's disease.
2. What are the early signs and symptoms?
Early symptoms of osteosarcoma include persistent bone pain that may worsen at night, swelling or tenderness near the affected area, and a lump or mass that feels warm to the touch.
3. Can osteosarcoma be cured?
The current multi-modal approach (combining chemotherapy and surgery) has improved long-term, disease-free survival rates to 60-70% for many patients.
4. Is osteosarcoma painful?
Yes, osteosarcoma can be painful. However, some osteosarcoma cases can be painless, especially in the early stages.
5. Can osteosarcoma recur after treatment?
Osteosarcoma can recur after treatment, typically within two to three years of completing initial therapy.
6. At what age does osteosarcoma develop?
Osteosarcoma most commonly affects people between the ages of 10 and 30, with a peak incidence during the teenage years.
7. Does osteosarcoma go away?
Osteosarcoma does not typically go away on its own. It requires aggressive treatment, usually involving a combination of chemotherapy and surgery.
8. How to detect osteosarcoma?
Osteosarcoma is typically detected through a combination of physical examination, imaging tests (X-ray, CT scan & MRI), and biopsy.
9. How long is chemo for osteosarcoma?
Chemotherapy for osteosarcoma usually lasts between 6 to 12 months. The osteosarcoma treatment typically involves cycles of chemotherapy before and after surgery. The exact duration can vary and depends on the individual case and treatment protocol.
10. Can osteosarcoma come back after surgery?
Yes, osteosarcoma can return after surgery. This is why chemotherapy is often given both before and after surgery to help reduce the risk of recurrence.
Still Have a Question?




