-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Osteoarthritis (OA)
Symptom, Causes, Diagnosis and Treatment
Osteoarthritis:
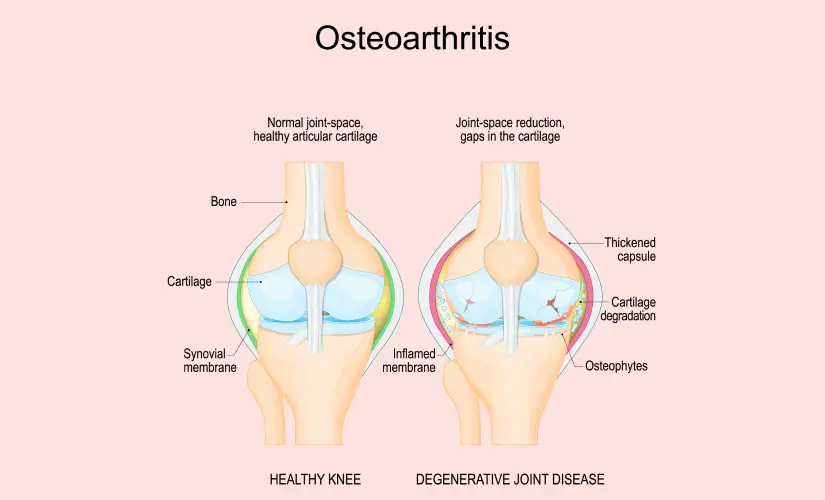
Osteoarthritis is a condition that affects the lives of millions, making every movement a challenge and turning routine tasks into daunting trials. As the most prevalent form of arthritis, understanding what causes osteoarthritis, its symptoms, and how it can be treated is crucial for maintaining a quality of life. This degenerative joint disease slowly wears away joint cartilage, leading to pain, stiffness, and swelling. Given its impact on everyday activities, finding effective treatment for osteoarthritis and engaging in osteoarthritis self-care are essential steps for managing this condition.
What is Osteoarthritis?
Osteoarthritis (OA) is a degenerative joint ailment in which the protective cartilage that cushions the ends of bones gradually wears down over time. It is the most common form of arthritis, affecting millions worldwide, especially older adults.
Types:
The following are two main types of osteoarthritis:
A. Primary Osteoarthritis: Primary OA is the most common form of the condition. It develops gradually over time due to normal joint wear and tear throughout one's life.
B. Secondary Osteoarthritis: Secondary osteoarthritis occurs when an underlying injury, trauma, or another condition directly damages the joint, leading to cartilage breakdown.
Stages of Osteoarthritis:
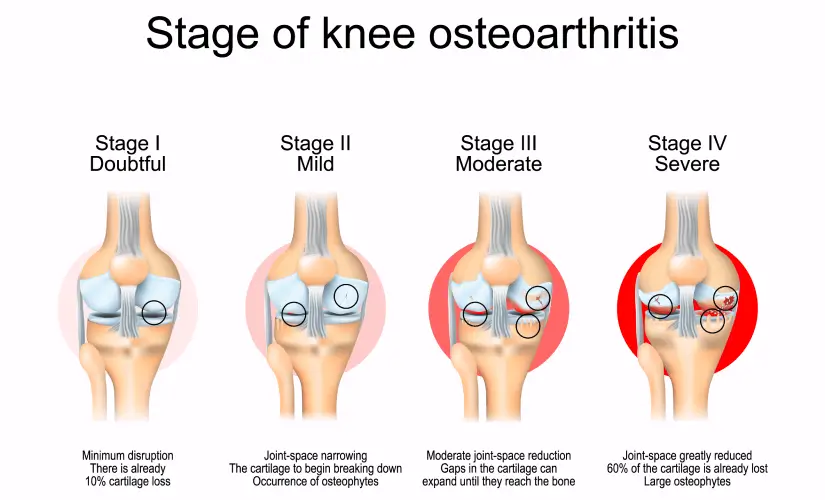
The most widely used system for classifying the stages of osteoarthritis is the Kellgren and Lawrence grading scale, which ranges from Grade 0 (no osteoarthritis) to Grade 4 (severe osteoarthritis).
Grade 0 (Normal)
Grade 1 (Doubtful)
Grade 2 (Minimal)
Grade 3 (Moderate)
Grade 4 (Severe)
Osteoarthritis Symptoms:
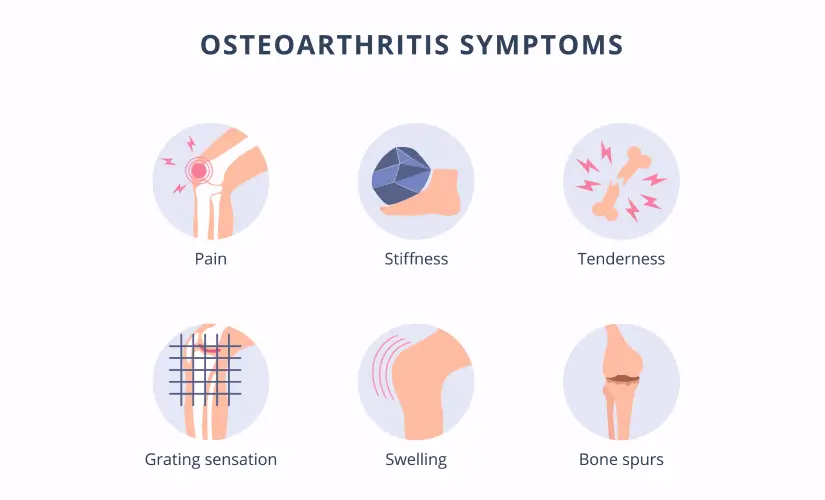
The symptoms of osteoarthritis often develop gradually and worsen over time. The most common signs and symptoms include:
- Pain and stiffness in the affected joint
- Tenderness
- Loss of Flexibility
- Grating Sensation
- Bone Spurs or extra bits of bone around the affected joint
- Swelling
- Joint Deformity
Osteoarthritis Causes:
While the exact causes of osteoarthritis are not fully known, researchers have pointed out several contributing factors that can increase the risk of developing the disease, such as:
- Age: As people age, the cartilage in their joints naturally wears down, making it more susceptible to damage.
- Obesity: Carrying excess body weight puts undue stress on weight-bearing joints (knees and hips), accelerating the breakdown of cartilage.
- Joint Injuries: Joint injuries, such as ligament tears, dislocations, and fractures, can increase the likelihood of developing osteoarthritis in that joint later in life.
- Overuse and Repetitive Stress: Certain occupations or activities that involve repetitive movements or excessive stress on a particular joint can increase the chance of osteoarthritis.
- Genetics: Some people may have a genetic predisposition to developing osteoarthritis
- Joint Deformities: Congenital or developmental abnormalities in joint structure can lead to improper weight and stress distribution within the joint, increasing the risk of osteoarthritis over time.
- Other Medical Conditions: Certain medical conditions, such as rheumatoid arthritis, gout, or metabolic disorders, can increase the likelihood of developing secondary osteoarthritis due to their impact on joint health and cartilage integrity.
How is Osteoarthritis Diagnosed?
Diagnosing osteoarthritis (OA) depends mainly on a symptoms review and a physical exam:
- Physical Examination: During the physical assessment, your doctor will check your affected joint for tenderness, swelling, redness, and flexibility. They analyse the extent of joint damage and identify any potential underlying causes.
- X-rays: Loss of the cartilage between joints shows up as a narrowing of the space between the bones, indicating osteoarthritis. An X-ray can also show bone spurs that can result from OA.
- Magnetic Resonance Imaging (MRI): An MRI may help identify cartilage damage and soft tissue tears that may affect joint stability and contribute to the development of OA.
- Ultrasound: Ultrasound, or sonography, may help view small changes in joint tissues, such as cysts, fluid buildup, cartilage thinning, bone spurs, or thickening of the synovium.
- Joint Fluid Analysis: Analysing the joint fluid can help rule out other possible conditions, such as gout or an infection.
How to Treat Osteoarthritis?
Various osteoarthritis treatment options are available for managing the symptoms of osteoarthritis and improving joint function. The treatment approach is typically customised to the person's needs and the severity of the condition, including:
Lifestyle Modifications:
- Exercise: Regular low-impact physical activity is crucial for maintaining joint flexibility, strengthening the muscles around the affected joints, and reducing pain.
- Weight Management: Losing extra pounds can substantially reduce the stress on weight-bearing joints (knees and hips) and alleviate pain and discomfort for obese people.
Medications:
- Over-the-counter pain reliever for mild to moderate osteoarthritis pain
- Both oral and topical NSAIDs can help reduce inflammation and relieve pain.
- Administration of corticosteroid injections into the affected joint can temporarily relieve pain and inflammation.
Physical and Occupational Therapy:
- Exercise Therapy: A physical therapist can design an exercise focusing on improving joint flexibility, strength, and range of motion.
- Manual Therapy: Massage, joint mobilisation, and stretching can help reduce pain and improve joint function.
- Assistive Devices: Occupational therapists can recommend assistive devices, such as canes, walkers, or braces, to help alleviate stress on the affected joints and improve mobility.
Alternative Therapies:
- Transcutaneous Electrical Nerve Stimulation (TENS): This therapy includes applying low-voltage electrical currents to the affected joint, which can help reduce pain perception.
- Viscosupplementation: Injections of hyaluronic acid into the affected joint can provide lubrication and cushioning, potentially reducing pain and improving joint function.
- Platelet-Rich Plasma (PRP) Therapy: In this therapy, doctors inject a concentration of the patient's own platelets into the affected joint to enhance healing and reduce inflammation.
- Cryoneurolysis: This minimally invasive procedure uses extreme cold to temporarily block nerve conduction, providing pain relief for knee osteoarthritis.
Surgical Interventions:
In severe cases where conservative approaches have been ineffective, surgical interventions may be considered:
- Joint Replacement Surgery (Arthroplasty): This procedure involves replacing the damaged joint with an artificial prosthetic joint, typically for the hip or knee.
- Osteotomy: This surgery involves realigning the bones around the affected joint to redistribute the weight and stress, potentially delaying joint replacement.
- Arthrodesis (Joint Fusion): In cases where joint replacement is not suitable, arthrodesis involves fusing the joint's bones together, eliminating joint movement and reducing pain.
Complications of Osteoarthritis:
- The primary complication is progressive joint pain and stiffness, which can become severe enough to hinder daily activities. As the condition worsens over time, individuals may experience chronic pain and disability, making simple tasks increasingly difficult.
- In advanced stages of osteoarthritis, cartilage and bone deterioration can lead to joint instability and deformity. This can cause further pain, discomfort, and functional limitations.
- Over time, osteoarthritis can cause thinning or tearing of the tendons and ligaments surrounding the affected joint, leading to joint instability and further complications.
- The repeated stress on the affected joint can lead to hairline cracks in the bone, known as stress fractures, which can cause additional pain and discomfort.
- Osteoarthritis can sometimes form soft, fluid-filled lumps behind the knee, known as Baker's cysts.
When to See a Doctor:
Additionally, seek medical guidance if you notice any of the following signs that your OA is worsening:
- Bony spurs or bumps on your joint
- Joint deformity or misalignment
- Joint locking, buckling, or instability
- Cracking, popping, or grinding sounds when moving the joint
How to Prevent Osteoarthritis?
Several lifestyle modifications can help reduce the possibility of developing osteoarthritis or slow its progression:
- Maintaining a healthy body weight
- Low-impact exercises like walking, swimming, or cycling
- Explore ways to reduce the strain on your joints
- Keeping diabetes under control and regulating blood sugar levels
- Avoid activities that stress the affected joint for at least 12 to 24 hours.
- A healthy, well-balanced meal rich in nutrients can promote overall joint health.
By adopting these preventive measures and making lifestyle changes, individuals can potentially reduce their risk of developing osteoarthritis or slow its progression, ultimately improving their quality of life.
Osteoarthritis vs Rheumatoid Arthritis (RA):
Osteoarthritis is a degenerative joint ailment that occurs when the smooth cartilage surrounding the bone ends wears down over time. It typically begins in an isolated joint, such as the knees, hips, or hands. The cartilage deterioration leads to bone-on-bone friction, causing pain, swelling, and reduced mobility.
On the other hand, RA is an autoimmune disorder in which the body's immune system mistakenly attacks the synovial membrane that lines and protects the joints. Unlike osteoarthritis, rheumatoid arthritis often targets multiple joints simultaneously, leading to symmetric joint involvement (e.g., arthritis in both hips or knees).
Conclusion:
While osteoarthritis is a challenging condition, individuals can find relief and maintain activity levels through informed choices and consistent care. Maintaining a healthy weight, staying active, and avoiding joint injuries are crucial preventive measures. Early osteoarthritis diagnosis and proactive management are vital to slowing disease progression and preserving joint function.
FAQs:
1) At what age does osteoarthritis usually start?
Ans: Osteoarthritis can develop at any age but is more common as people age older.
2) What is the best thing to do for osteoarthritis?
Ans: There is no single best treatment for osteoarthritis, as the management approach depends on the severity of the condition and individual factors. However, some of the recommended strategies include:
- Regular exercise
- Maintaining a healthy weight
- Over-the-counter medications or topical creams for pain relief.
- Physical therapy helps improve joint function and mobility.
3) What should you not do with osteoarthritis?
Ans: Avoid high-impact exercises or activities, prolonged periods of inactivity or immobility, excessive weight, and ignoring pain or pushing through severe joint pain during activities.
4) Is osteoarthritis curable?
Ans: No, osteoarthritis is not a curable condition. However, various treatments and lifestyle modifications can slow disease advancement and improve joint function and quality of life.
5) Is walking good for osteoarthritis?
Ans: Walking is a low-impact physical activity. It strengthens the muscles around the knee joints, improves joint flexibility, and reduces pain & stiffness.

Still Have a Question?



