-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Interstitial Cystitis
Symptom, Causes, Diagnosis and Treatment
Interstitial Cystitis
Chronic bladder pain affects millions of people worldwide, significantly impacting their daily lives. For many, this persistent discomfort stems from a condition called interstitial cystitis, also known as bladder pain syndrome. Persistent pelvic pain and frequent and urgent urination can affect work, relationships, and social activities due to discomfort and unpredictability. This comprehensive guide explores interstitial cystitis's types, symptoms, and causes.
What is Interstitial Cystitis?
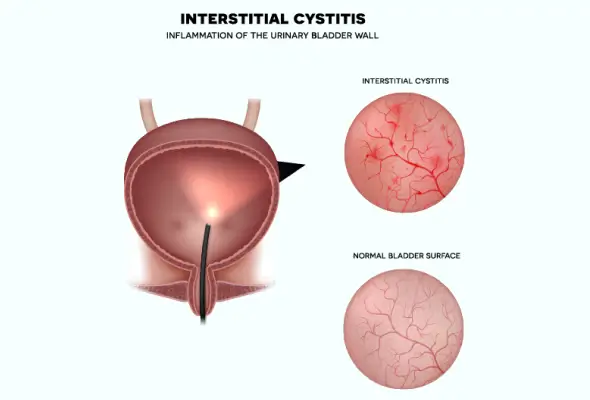
Interstitial cystitis is a chronic condition that affects the bladder wall, causing inflammation and irritation. The term "interstitial" refers to the spaces between tissues or organs, while "cystitis" indicates bladder inflammation. This condition can lead to scarring and stiffening of the bladder walls, reducing its capacity to hold urine.
Doctors often refer to this condition by several names:
- Bladder pain syndrome (BPS)
- Painful bladder syndrome
- Frequency-urgency-dysuria syndrome
- Chronic pelvic pain
The condition primarily affects the protective lining (epithelium) of the bladder. When this protective barrier becomes compromised, toxic substances in urine can irritate the bladder wall, leading to chronic discomfort and pain. This damage to the bladder wall can create a cycle of symptoms that significantly impact daily life.
Types of Interstitial Cystitis
Medical experts have identified two distinct interstitial cystitis (IC) types, each with unique characteristics and treatment approaches.
- Ulcerative Interstitial Cystitis: Ulcerative IC affects approximately 5-10% of patients. This form is characterised by Hunner's ulcers, which are painful sores that develop on the bladder wall. These ulcers can cause significant discomfort and may require specific targeted treatments to manage symptoms effectively.
- Non-ulcerative Interstitial Cystitis: Non-ulcerative IC affects about 90% of cases. This variation presents with tiny haemorrhages called glomerulations on the bladder wall. While these minor bleeding points might not be visible to the naked eye, doctors can identify them during medical examination procedures.
Symptoms of Interstitial Cystitis
Common symptoms include:
- Persistent pain or pressure in the pelvic area
- Frequent urination (up to 60 times daily)
- Urgent need to urinate, even after vacating the bladder
- Discomfort that worsens as the bladder fills
- Pain relief after urinating
- Pain during sexual activity
- Small amounts of urine output despite frequent urination
The condition can significantly impact daily life, affecting sleep patterns, work productivity, and social relationships. Many individuals find themselves planning activities around bathroom accessibility, and some may experience difficulties maintaining intimate relationships due to pain during or after sexual activity.
Causes of Interstitial Cystitis
Current scientific evidence suggests that multiple factors trigger bladder pain interstitial cystitis condition.
A significant finding indicates a potential defect in the bladder's protective lining (epithelium). When this protective barrier becomes compromised, it can allow toxic substances in urine to penetrate and irritate the bladder wall, leading to the characteristic symptoms of bladder pain syndrome.
Scientists have identified several potential contributing factors that may play a role in developing interstitial cystitis:
- Autoimmune Response: The body's immune system may mistakenly attack the bladder tissue
- Genetic Predisposition: Family history suggests hereditary factors
- Nerve Dysfunction: Changes in the nerves that carry bladder sensations
- Mast Cell Activation: Abnormal immune cells causing allergic reactions
- Environmental Triggers: Including infections or injuries to the bladder
- Vascular Disease: Problems with blood vessels in the bladder
Risk Factors
Research has identified specific groups that face a higher risk of developing interstitial bladder pain:
- Gender: Women are significantly more susceptible to receiving an interstitial cystitis diagnosis compared to men
- Age: Most diagnoses occur in people aged 30 or older
- Physical Characteristics: Individuals with fair skin and red hair show a higher predisposition
- Chronic Pain Conditions: People with existing conditions like fibromyalgia or irritable bowel syndrome face increased risk
- Mental Health: Those with depression or anxiety disorders show higher susceptibility
Complications of Interstitial Cystitis
One of the most significant physical complications is reduced bladder capacity. The continuous inflammation can cause the bladder wall to become stiff and rigid, limiting the amount of urine it can hold. This physical change forces people to visit the bathroom more frequently, disrupting their daily activities.
The impact of interstitial cystitis extends beyond physical symptoms, affecting multiple aspects of life:
- Disrupted sleep patterns due to frequent urination
- Difficulty maintaining regular work schedules
- Limited social activities and travel
- The strain on personal relationships
- Increased risk of anxiety and depression
- Reduced self-esteem
- Social embarrassment
- Sexual intimacy challenges
Diagnosis
Doctors often ask patients to maintain a bladder diary, recording fluid intake and urination patterns. This helps establish baseline symptoms and identify potential triggers.
Doctors employ several diagnostic tools to confirm interstitial cystitis:
- Urinalysis and Culture: Tests urine samples for infection or other abnormalities
- Pelvic Examination: Checks for tenderness or abnormalities in the pelvic region
- Cystoscopy: Here, the clinician uses a thin tube with a camera to examine the bladder lining
- Bladder Biopsy: Removes small tissue samples to rule out other conditions
- Potassium Sensitivity Test: Measures bladder sensitivity to different solutions
Interstitial Cystitis Treatment
The treatment for bladder cystitis typically involves a combination of approaches:
- Lifestyle Modifications:
- Dietary changes to avoid trigger foods, such as alcohol, caffeine, carbonated beverages, fruit juices, chocolates, and artificial sweeteners
- Stress reduction techniques like yoga or psychotherapy
- Regular gentle exercise
- Bladder training exercises
- Medical Interventions:
- Oral medications, including anti-inflammatory drugs
- Physical therapy focusing on pelvic floor muscles
- Nerve stimulation treatments
- Bladder instillations with medication
When to See a Doctor
Doctors recommend scheduling an appointment if any of these symptoms persist:
- Bladder pain lasting more than six weeks
- Frequent urination that disrupts daily activities
- Urgent need to urinate despite empty bladder
- Pain that doesn't respond to over-the-counter medications
- Discomfort during or after sexual activity
Prevention
People living with bladder pain syndrome can implement several practical approaches to reduce the likelihood of symptom recurrence:
- Food Journal Maintenance: Keeping detailed records of dietary choices and their effects on symptoms helps identify trigger foods
- Treatment Consistency: Following prescribed treatment plans even during symptom-free periods
- Stress Management: Implementing relaxation techniques and lifestyle adjustments to minimise stress levels
- Regular Exercise: Engaging in gentle physical activities that don't aggravate symptoms
- Environmental Control: Creating comfortable surroundings that support bladder health
Conclusion
Living with interstitial cystitis presents unique challenges, but proper understanding and management can significantly improve quality of life. Medical science continues to advance treatment options, offering multiple approaches, from lifestyle changes to medical interventions.
People affected by this condition benefit most from early diagnosis and personalised treatment plans. Doctors now recognise that successful management often requires a combination of approaches, including dietary modifications, stress management, and medical treatments tailored to individual needs.
FAQs
1. Is interstitial cystitis curable?
While interstitial cystitis cannot be completely cured, proper treatment can effectively manage it. Many patients experience improvement in their symptoms through medications, lifestyle changes, and other therapeutic approaches. The key lies in identifying the right treatment combination that works for each individual.
2. Can cystitis damage your kidneys?
Interstitial cystitis itself does not typically cause kidney damage. However, recurring urinary tract infections, which can sometimes be confused with IC, may lead to kidney problems if left untreated.
3. How long can interstitial cystitis last?
Interstitial cystitis is a chronic condition that typically requires ongoing management throughout a person's life. Many people experience periods of remission where symptoms associated with interstitial cystitis improve or disappear, followed by flares when symptoms return. The duration and intensity of symptoms vary significantly among individuals.
4. What is stage 4 interstitial cystitis?
Stage 4 interstitial cystitis represents an advanced condition where the bladder tissue becomes hardened and can only hold small amounts of urine. This stage affects approximately 5% of IC patients and typically occurs after two or more years of continuing symptoms. The bladder's reduced capacity often leads to more frequent urination and increased pain.
5. Who does interstitial cystitis affect?
Interstitial cystitis can affect anyone, but certain groups face higher risk:
- Women are diagnosed more frequently than men
- Most diagnoses occur in people aged 30 or older
- Individuals with other chronic pain conditions show increased susceptibility
Dr. Vaibhav Vinekar

Still Have a Question?



