-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Herpangina
Symptom, Causes, Diagnosis and Treatment
Herpangina
Herpangina, a highly contagious viral infection, mainly affects children under 10 years of age and can cause alarming fevers reaching up to 106°F (41.1°C). Let's explore the essential aspects of herpangina, from its causes and symptoms to herpangina cure and preventive measures. Readers will learn how to identify the condition, understand its progression and know when to seek medical attention for their children.
What is Herpangina?
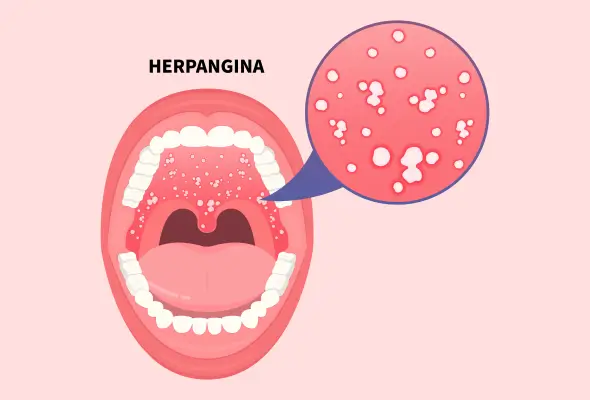
A viral infection primarily targeting the oropharynx, herpangina presents as small blister-like ulcers at the back of the throat and roof of the mouth. The condition is a significant health concern, notably affecting toddlers and children below 10. Herpangina typically resolves within a week without complications, but medical attention may be necessary in severe cases.
Symptoms of Herpangina
The onset of herpangina symptoms typically occurs 3-5 days after exposure to the virus.
Initial symptoms often mirror those of common viral infections, starting with:
- A sudden onset of fever, sometimes reaching up to 106°F (41°C)
- Persistent headache
- Swollen lymph glands
- Neck pain
- Sore throat with pain while swallowing
The most distinctive feature of herpangina emerges as small, blister-like bumps in specific areas of the mouth. These sores commonly appear:
- On the roof of the mouth
- At the back of the throat
- On the tonsils
- On the uvula
- On the tongue
These blisters initially present as light red spots, measuring less than half a centimetre across. As the condition progresses, they develop into ulcers characterised by a light grey colour surrounded by a red border.
The presence of these painful sores leads to several secondary symptoms:
- Difficulty in swallowing
- Decreased appetite
- Increased drooling
- Fussiness, particularly in young children
Some children might experience additional symptoms based on the specific virus causing the infection. These can include:
- Muscle weakness
- Breathing difficulties
- Back pain (more common in older children)
- Vomiting
One significant concern associated with herpangina is the risk of dehydration. This occurs primarily because the mouth and throat pain often leads to reduced fluid intake. Signs of dehydration include:
- Increased fatigue
- Decreased urination frequency
- Persistent dry mouth
Risk Factors and Causes of Herpangina
Several highly contagious viruses trigger herpangina, with Coxsackieviruses A and B being the primary culprits. Echovirus and Enterovirus 71 also contribute significantly to causing this condition.
The transmission of herpangina occurs through multiple pathways:
- Close physical contact with infected individuals
- Inhalation of respiratory droplets
- Direct exposure to bodily fluids, including saliva and mucus
- Contact with contaminated faecal matter
The virus demonstrates a three to five-day incubation period between exposure and symptom onset. Infected individuals remain contagious for three to eight weeks following the incubation period, with peak infectivity occurring during the initial two weeks.
Certain groups face heightened vulnerability to herpangina:
- Children under 10 years, particularly those attending daycare or school
- Newborns
- Individuals with compromised immune systems
- Pregnant women
Complications of Herpangina
Dehydration is the most frequent complication, primarily due to painful swallowing that discourages fluid intake. Signs of dehydration in children include:
- Dry mouth and reduced tear production
- Sunken eyes and decreased urination
- Unusual sleepiness or irritability
- Sunken soft spot on infants' heads
Specific strains of the virus, particularly enterovirus 71, might lead to severe neurological complications requiring immediate medical intervention. These complications include:
- Brain stem encephalitis
- Acute flaccid paralysis
- Aseptic meningitis
- Myocarditis
In infants, these complications encompass liver failure and inflammation of the brain tissues. The condition rarely proves fatal, yet when deaths occur, they predominantly affect infants under one year of age.
Diagnosis of Herpangina
- Clinical History: Doctors begin the diagnostic process by gathering detailed information about:
- Current symptoms
- Medical history
- Recent exposure to infected individuals
- Seasonal timing of symptoms
- Physical Assessment: Physical examination reveals characteristic ulcers in specific locations:
- Posterior pharynx region
- Soft palate area
- Anterior tonsillar pillars
- Laboratory Analysis: Laboratory testing becomes necessary solely in specific circumstances:
- Cases involving complications
- During disease outbreaks for epidemiological data
- Situations requiring differentiation from severe conditions
- Additional Tests: In cases where testing proves essential, several methods exist:
- Enterovirus isolation through cell culture (gold standard)
- Polymerase chain reaction (PCR) testing
- Enzyme-linked immunosorbent assays (ELISA)
- Serum antibody measurements
- PCR testing offers superior advantages, delivering swift and precise results.
- Blood tests typically show normal white blood cell counts, yet lymphocytosis might occur occasionally. Serum antibody measurements require two samples taken 2-3 weeks apart, showing a four-fold rise in antibody levels.
Herpangina Treatment
Since herpangina stems from viral infections, doctors focus primarily on managing symptoms and ensuring patient comfort throughout the recovery period.
- Herpangina Medications: Topical treatments offer localised relief from mouth sores and throat pain. These include:
- Lidocaine-based anaesthetic solutions
- Therapeutic salt water rinses after meals
- Soothing mouth sprays and gels
- Throat lozenges (for children aged six and above)
- Fluid Management: Proper hydration plays a vital role in recovery. Recommended fluids encompass:
- Cold dairy products
- Electrolyte beverages
- Ice cream or popsicles
- Water
- Dietary Modifications: Soft, bland foods support recovery whilst minimising discomfort. Patients should avoid:
- Hot beverages
- Acidic foods and drinks
- Spicy dishes
- Salty snacks
- Fried items
Rest remains fundamental for recovery. Patients should isolate themselves in well-ventilated rooms to minimise virus transmission.
When to See a Doctor
Medical assistance becomes crucial upon noticing these warning signs:
- Fever reaching above 106°F (41°C) lasting more than five days
- Inability to drink or eat for 24 hours
- Mouth sores persisting beyond one week
- Vomiting or diarrhoea extending past 24 hours
Dehydration stands as a primary concern requiring swift medical intervention.
Preventions of Herpangina
Regular handwashing is the cornerstone of prevention, proving vital in reducing viral transmission. Proper hand hygiene becomes essential after:
- Changing diapers
- Using the bathroom
- Feeding children
- Handling contaminated items
Maintaining a clean environment plays a crucial role in prevention. This includes sanitising frequently touched surfaces and objects throughout the home. Areas requiring particular attention encompass:
- Door handles
- Remote controls
- Drawer pulls
- Refrigerator handles
Families caring for infected individuals should implement specific preventive measures. The affected person needs isolation in a well-ventilated room until symptoms improve.
Conclusion
Herpangina remains a manageable condition despite its uncomfortable symptoms and highly contagious nature. Though the infection primarily affects young children, proper understanding and prompt action can significantly reduce its impact on daily life. Parents and caregivers should remember that most cases resolve naturally within 7-10 days without serious complications.
Careful attention to hydration, pain management, and proper rest proves essential throughout the recovery period. Doctors emphasise that while antibiotics offer no benefit against this viral infection, following recommended dietary guidelines and maintaining good hygiene practices helps prevent its spread.
FAQs
1. How common is herpangina?
Herpangina frequently surfaces in babies and children under 10 years old, with peak occurrence during the summer and autumn months. The condition demonstrates heightened activity in educational settings, spreading swiftly through daycare centres and schools where children maintain close contact.
2. How does herpangina affect a child's body?
The virus impacts multiple body systems, causing small blister-like bumps in the mouth, primarily affecting the back of the throat and roof of the mouth. These painful sores often lead to decreased appetite and difficulty swallowing. Children might experience muscle weakness, breathing difficulties, and, in some instances, back pain. The condition typically triggers high fevers reaching 106°F (41°C).
3. How long does herpangina last?
Most children experience symptom improvement within 7-10 days. Throughout this period, infected individuals remain contagious, potentially spreading the virus for three to eight weeks after initial infection. The incubation period typically spans 3-5 days between exposure and symptom onset.
4. What foods are good for herpangina?
Specific foods aid recovery and provide comfort:
- Soft, bland proteins:
- Ground meats
- Scrambled eggs
- Chicken salad
- Soothing dairy products:
- Cold milk
- Plain yoghurt
- Ice cream
- Gentle carbohydrates:
- Soft breads
- Cooked cereals
- Mashed potatoes
Patients should avoid acidic, spicy, or hot foods that might irritate mouth sores.
Still Have a Question?


