-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Guillain-Barre Syndrome
Symptom, Causes, Diagnosis and Treatment
Guillain-Barre Syndrome
Guillain-Barre syndrome affects about 100,000 people worldwide each year. This rare but debilitating autoimmune disorder can strike without warning. People between 30 and 50 years of age develop Guillain Barre disease symptoms rapidly over days or weeks. The recovery outlook brings hope as majority of patients recover within six months after symptoms appear. A full recovery might sometimes take several years. In this comprehensive blog, let us explore what GBS is, its causes, diagnosis, and different treatment modalities.
What is Guillain-Barre syndrome (GBS)?
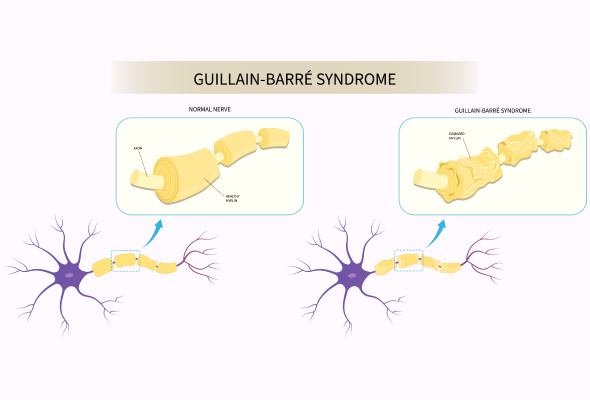
GBS creates a unique challenge for the peripheral nervous system that controls muscle movement and those that help you feel pain, temperature, and touch. The body’s immune system attacks its own nerves by mistake. This rare neurological disorder stands as the leading cause of acute flaccid paralysis in many parts of the world.
People with GBS first notice weakness and tingling in their hands and feet. Anyone who shows signs of GBS needs medical help right away because symptoms can get worse quickly. Here is what one needs to know about GBS:
- Symptoms can show up within days or take several weeks to appear
- Men get GBS more often than women, at a ratio of 1.5:1
- The condition affects people of all ages, but more often in men between 30-50 years
- Most cases start after a viral or bacterial infection
Research shows that about two-thirds of patients notice symptoms six weeks before onset of GBS. These infections range from breathing problems to stomach issues. Most patients see major improvements within six months after symptoms start. Some people might still feel weak, numb, or tired after recovery.
Guillain-Barre Syndrome Types
Research has revealed several distinct types of Guillain-Barre syndrome (GBS) that affect the nervous system in different ways.
- Acute Inflammatory Demyelinating Polyneuropathy (AIDP): This variant affects the myelin sheaths of nerves, and weakness begins in the lower body before moving upward.
- Acute Motor Axonal Neuropathy (AMAN): This type only affects movement-linked nerves, often linked to infections like Campylobacter jejuni.
- Acute Motor-Sensory Axonal Neuropathy (AMSAN): This severe variant affects both movement and sensory nerves, causing widespread paralysis and sensory disturbances with a prolonged recovery time.
- Miller-Fisher syndrome (MFS): This type is characterised by ophthalmoplegia, ataxia, and areflexia, often without significant limb weakness
Symptoms of Guillain-Barre Syndrome
The primary symptom of Guillain-Barre syndrome is tingling and weakness in the feet and legs. These sensations move up through the body and affect the upper body and arms.
Symptoms progress in a clear sequence:
- Pins and needles sensations in toes, fingers, ankles or wrists
- Muscle weakness that spreads from the legs to the upper body
- Difficulty with walking or climbing stairs
- Problems with facial movements, including speaking and swallowing
- Vision issues, including double vision
- Severe pain that intensifies at night
- Loss of Bladder and bowel control
- Changes in heart rate and blood pressure
- Breathing problems
Patients reach peak weakness within two weeks after their first symptoms. About 90% of patients reach their most severe stage by week three.
Causes of GBS Disease
Research has found that Guillain-Barre syndrome develops after an infection sets off an unusual response from the immune system. About 70% of patients show symptoms between one to six weeks after they get sick. The immune system attacks peripheral nerves by mistake in this condition. The body's defense mechanisms can damage myelin, the protective covering of nerves. This blocks the vital communication between the brain and muscles.
Risk Factors
People can develop Guillain-Barre syndrome due to several factors. These include:
- Bacterial infections, mostly Campylobacter jejuni
- Viral infections like cytomegalovirus, Epstein-Barr virus, and Zika virus
- Recent surgical procedures
- Respiratory or gastrointestinal infections within the
- previous six weeks
- Advanced age, especially in those above 50 years
- Male gender, with slightly higher occurrence rates
- Recent lung infections or bacterial gastroenteritis
Complications of Guillain-Barre Syndrome
Guillain-Barre syndrome can cause mild to severe complications that affect the autonomic nervous system. The condition can lead to several other problems:
- Breathing difficulty
- Irregular heart rhythms
- Trouble with digestion and bladder control
- Blood clots from not moving enough
- Bed sores from lying down too long
- Ongoing nerve pain in one of every three patients
- Lingering numbness and tingling feelings
- A small number of patients experience relapses
Diagnosis of Guillain-Barre syndrome
Careful assessment of Guillain-Barre syndrome is essential because its symptoms resemble other neurological conditions.
The diagnostic process starts with a review of the patient's medical history and recent illnesses. GBS usually develops after an infection, so doctors search for evidence of previous illness in the last six weeks. The classic diagnostic pattern shows progressive, symmetrical weakness, among other signs like decreased or absent reflexes. They check muscle strength and reflexes during physical examinations.
Several key tests help doctors confirm the diagnosis:
- Spinal Tap (Lumbar Puncture): This test shows increased protein levels in cerebrospinal fluid
- Nerve Conduction Studies: To assess nerve function
- Electromyography (EMG): Thin-needle electrodes inserted into muscles help assess muscle and nerve function.
Doctors track the progression of the condition through repeated neurological examinations.
Treatment for GBS Syndrome
Patients with Guillain-Barre syndrome need to be admitted to the hospital right away to get treatment and close monitoring. The medical team works on two fronts: stop the immune system from attacking nerves and provide supportive care until the patient starts recovering.
The following are common GBS disease treatment approaches:
- Plasma Exchange (Plasmapheresis): A machine separates plasma from blood cells, filters out harmful antibodies, and returns treated blood to the body
- Immunoglobulin Therapy (IVIG): Healthy antibodies from blood donors block the damaging antibodies causing GBS
- Medications: Medicines to control severe pain and prevent blood clots
- Physical Therapy: To improve movement of arms and legs
- Speech and swallow Therapy: Helps those who have trouble swallowing
When to See a Doctor
You should seek urgent medical help if you experience:
- Tingling that starts in feet or toes and moves upward through the body
- Weakness that spreads faster
- Difficulty breathing, especially while lying flat
- Problems with swallowing or choking on saliva
- Sudden muscle weakness that gets worse over hours or days
GBS patients need immediate hospital care because symptoms can get worse quickly.
Prevention
Medical science cannot guarantee the complete prevention of Guillain-Barre syndrome. You can take several basic hygiene steps to reduce your risk of developing this condition. A strong immune system is your first defense against potential triggers.
These simple preventive measures help:
- Regular hand washing with mild soap and water, especially after bathroom visits and before food handling
- Proper cooking of meat to avoid Campylobacter jejuni infections
- Staying away from people with contagious respiratory or stomach infections
- Keeping common surfaces clean and disinfected, including tables, door handles, and phones
- Maintaining up-to-date vaccination records
- Following good food safety practices to prevent cross-contamination
- Your immune system benefits from a balanced diet rich in fruits, vegetables, lean proteins, and whole grains.
- Physical activity and adequate sleep play significant roles in maintaining overall health.
- Your body's natural defenses grow stronger when you manage stress levels through proper rest and exercise.
- Seek prompt medical attention if symptoms like fever, diarrhoea, or respiratory issues appear.
- Better public awareness about early warning signs leads to faster diagnosis and management, which reduces the chance of serious outcomes.
Conclusion
Guillain-Barre syndrome is a rare neurological condition that requires prompt medical intervention. Modern medical treatments have greatly improved patient outcomes through plasma exchange and immunoglobulin therapy. Most patients can walk again within six months of treatment, though recovery times vary.
Recovery needs both patience and proper medical support. A patient's recovery prospects improve with immediate medical attention after the first symptoms appear. The combination of physical therapy and appropriate medical treatments helps patients build their strength back and become independent.
FAQs
1. Is GBS a serious disease?
Yes, GBS can be serious and potentially life-threatening. However, with proper treatment, most people recover fully.
2. How long does GBS last?
The acute phase of GBS typically lasts a few weeks, but recovery can take months to years. Most people show significant improvement within 6-12 months.
3. What is the root cause of GBS?
The exact reason is unknown, but doctors believe it to be an autoimmune response triggered by infections or, rarely, other factors like infection, surgery or vaccinations.
4. Can you fully recover from Guillain-Barre syndrome?
Most people recover fully from GBS, even from severe cases. However, about 30% of adults may have some residual weakness after three years.
5. Is it bad to be GBS-positive?
Being Guillain-Barre syndrome (GBS) positive means your immune system is attacking your nerves, causing weakness and paralysis. While serious, early treatment can improve recovery, though some may have lasting effects.
6. What antibiotic kills GBS?
Antibiotics are not used to treat Guillain-Barre syndrome as bacteria do not cause it. Treatment mainly focuses on managing GBS symptoms and supporting the immune system.
7. Who is most at risk for GBS?
Adults between 30 to 50 years of age and males are slightly more at risk, but GBS can affect people of all ages and genders.
8. Can you live a normal life with Guillain-Barre syndrome?
Most people return to normal activities after recovering from GBS. Some may experience lasting effects, but many achieve a full recovery with time and rehabilitation.
9. How is GBS transmitted?
GBS is not contagious or transmitted from person to person. It’s an autoimmune response, often triggered by an infection.
10. What foods are good for GBS?
While no specific diet is proven to treat GBS, a balanced, nutritious diet can support overall health during recovery. Consult with a doctor for personalised dietary advice.
11. What foods should you avoid with Guillain-Barre syndrome?
There are no specific foods known to worsen GBS. However, maintaining a healthy dietary habit and staying hydrated is essential during recovery.
12. What can happen if GBS is not treated?
Untreated GBS can lead to severe complications, including respiratory failure, cardiac issues, and long-term nerve damage. Prompt treatment is essential for the best outcomes.

Still Have a Question?



