-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Glomerulonephritis
Symptom, Causes, Diagnosis and Treatment
Glomerulonephritis
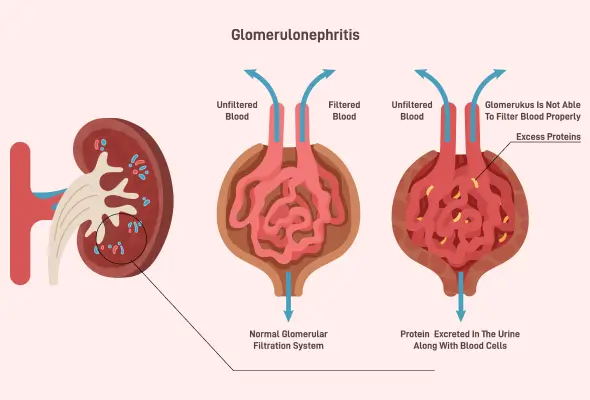
The kidneys filter about one hundred and fifty quarts of blood every day, keeping the body free from waste and excess fluid. Glomerulonephritis kidney disease occurs when the tiny filtering units in the kidneys, called glomeruli, become inflamed and damaged. Understanding its causes, recognising early warning signs, and seeking proper medical care are essential steps in managing this condition effectively.
What Is Glomerulonephritis?
Glomerulonephritis is a complex kidney disease characterised by inflammation of the tiny filtering units called glomeruli. These microscopic structures, nearly one million within each kidney, act as sophisticated filtration devices that clean the blood of waste products & excess fluid.
When glomerulonephritis kidney disease develops, it can manifest in two distinct forms:
- Acute Glomerulonephritis: Develops suddenly and may resolve with proper treatment
- Chronic Glomerulonephritis: Progresses slowly over time and can lead to permanent kidney damage
IgA nephropathy stands as the most prevalent form of glomerulonephritis worldwide. The condition can occur independently or as part of other diseases, such as lupus or diabetes. Without timely intervention, glomerulonephritis often becomes progressive, potentially leading to chronic kidney disease and associated cardiovascular complications.
Symptoms of Glomerulonephritis
Many people with glomerulonephritis kidney disease do not experience any warning signs, but some may experience certain symptoms, such as:
- Pink or cola-coloured urine due to blood presence
- Foamy or bubbly urine caused by excess protein
- Swelling in the face, hands, feet, and abdomen
- Changes in urination frequency
- High blood pressure
- Nausea and vomiting
- Muscle cramps and fatigue
- Joint or abdominal pain
- Shortness of breath
- Unexplained weight loss
Causes and Risk Factors of Glomerulonephritis
The leading causes of glomerulonephritis include:
- Infections:
- Post-streptococcal infection following strep throat
- Bacterial endocarditis affecting heart valves
- Viral infections, including hepatitis B, hepatitis C, and HIV
- Autoimmune Conditions:
- Lupus- affecting multiple body systems
- Goodpasture's syndrome- impacts the lungs and kidneys
- IgA nephropathy with antibody deposits in glomeruli
- Blood Vessel Disorders:
- Polyarteritis affecting medium and small blood vessels
- Granulomatosis with polyangiitis impacting multiple organs
- Sclerotic Conditions:
- Long-term high blood pressure
- Diabetic kidney disease
- Focal segmental glomerulosclerosis
Several factors increase the likelihood of developing glomerulonephritis. These include:
- Personal or family history of kidney disease
- Exposure to certain medications or toxins
- Presence of autoimmune conditions
Complications of Glomerulonephritis
The breakdown in kidney function can result in:
- Accumulation of waste products in the blood
- Poor regulation of essential minerals
- Loss of red blood cells
- Decreased protein levels in the blood
Serious complications can develop over time, such as:
- Acute kidney failure
- Chronic kidney disease, characterised by declining kidney function over three or more months
- End-stage kidney disease
- High blood pressure from damaged glomeruli and nephrotic syndrome, where excessive protein loss through urine leads to low blood protein level
Diagnosis
Doctors typically prescribe these essential diagnostic tests:
- Urine Analysis: Tests reveal the presence of red blood cells, proteins, and white blood cells that indicate inflammation. The appearance of red blood cell casts strongly suggests glomerulonephritis.
- Blood Tests: These measure waste product levels, check for antibodies, and assess complement levels. Investigations include complete blood count (CBC), blood urea nitrogen (BUN), and serum creatinine measurements.
- Imaging Studies: Ultrasound, X-rays, or CT scans help evaluate kidney size and shape while checking for structural abnormalities or blockages.
- Kidney Biopsy: This definitive test involves removing a small piece of kidney tissue using a special needle. The sample undergoes microscopic examination to confirm the diagnosis & determine the type and extent of damage.
Treatment
The main glomerulonephritis treatment strategies include:
- Medication Management:
- Immunosuppressants to control immune system response
- Blood pressure medications like ACE inhibitors
- Steroids to reduce inflammation
- Diuretics to manage fluid retention
- Immunisation:
- Vaccinations against flu and pneumonia are recommended for patients, as the condition can increase vulnerability to infections.
- Home Remedies:
- Natural Support options include carrot juice mixed with honey & fresh lime juice in the morning. However, patients should avoid certain substances that can strain the kidneys, including alcohol, excessive caffeine, and foods high in oxalates like chocolate and spinach.
When to See a Doctor
Individuals should contact their doctor immediately if they notice:
- Blood in urine or changes in urine appearance
- Unexplained swelling in the face or legs
- Shortness of breath
- Changes in urination frequency
- Severe joint pain
Prevention
Essential preventive measures include:
- Maintaining strict blood pressure control through medication and lifestyle changes
- Managing diabetes effectively with proper blood sugar monitoring
- Following a balanced diet with reduced salt intake
- Practising good hygiene and safe sex to prevent infections
- Getting seasonal flu and pneumococcal vaccines
- Using over-the-counter pain medications only as directed
- Avoiding smoking or quitting if currently smoking
Conclusion
The combination of medical treatments, dietary changes, and preventive measures offers hope for patients dealing with this glomerulonephritis. Regular monitoring, medication adherence, and lifestyle adjustments help slow disease progression and maintain kidney function. Doctors stress that each patient's journey with glomerulonephritis differs, making personalised treatment approaches essential for optimal outcomes.
FAQS
1. How do glomeruli help your kidneys?
Glomeruli are microscopic filtering units in the kidneys, with nearly a million of them working continuously. These tiny structures act as sophisticated filters, removing waste products & excess fluid from the blood while retaining essential proteins and cells needed for healthy body function.
2. Is glomerulonephritis a serious disease?
Yes, glomerulonephritis requires careful medical attention as it can lead to kidney issues if left untreated. The condition may become chronic kidney disease or kidney failure in some cases, making early detection and proper treatment essential for better outcomes.
3. What is the difference between nephritic syndrome and glomerulonephritis?
While glomerulonephritis specifically refers to inflammation of the kidney's filtering units, nephritic syndrome describes a collection of symptoms that can result from this inflammation. Key differences include:
- Nephritic syndrome focuses on specific symptoms like blood in urine and high blood pressure
- Glomerulonephritis describes the underlying kidney condition causing these symptoms
4. Is glomerulonephritis curable?
The curability of glomerulonephritis depends on the underlying cause. Some forms, particularly those following streptococcal infections, may improve with proper treatment. Chronic cases typically require ongoing management to prevent further kidney damage and maintain kidney function.
5. What foods are good for glomerulonephritis?
A kidney-friendly diet typically includes:
- Fresh fruits and vegetables low in potassium
- Lean proteins in moderate amounts
- Whole grains and unprocessed foods
- Foods low in sodium and phosphorus
6. Who treats glomerulonephritis?
A kidney specialist (nephrologist) typically leads the treatment team. They work alongside primary care physicians and other specialists to develop comprehensive treatment plans tailored to each patient's conditions and needs.
To Book an Appointment, call:
Still Have a Question?




