-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Folliculitis
Symptom, Causes, Diagnosis and Treatment
Folliculitis
Folliculitis affects millions worldwide, causing uncomfortable inflammation in hair follicles anywhere on the body. Many people mistake folliculitis for common acne or other skin problems, making proper identification crucial for effective folliculitis treatment. This article explores the different types of folliculitis, its causes, available treatments, and prevention strategies to help readers recognise, treat, and prevent future outbreaks.
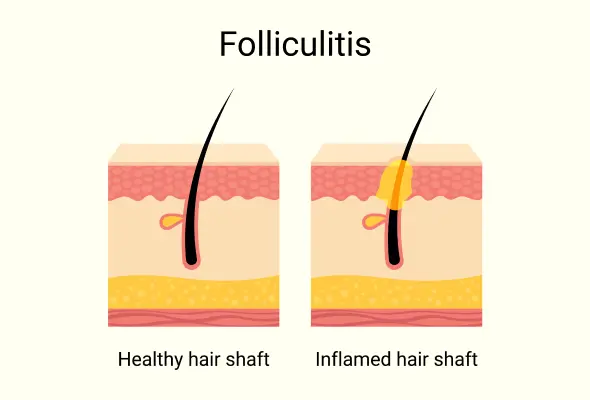
What is Folliculitis?
It is a common skin condition characterised by inflammation or infection of hair follicles, the tiny pockets from which hair grows. This condition manifests as small, pus-filled blisters or red bumps around hair follicles, which can develop on any body part where hair grows.
While folliculitis is generally a benign condition that often resolves on its own with basic self-care, it can present significant challenges for people with compromised immune systems. The condition can develop from everyday activities such as shaving, using hot tubs, or excessive sweating during exercise or outdoor work.
Types of Folliculitis
The most common types of folliculitis include:
- Bacterial Folliculitis: Caused by Staphylococcus aureus bacteria, presenting as small, red or white pus-filled pimples that typically resolve within days.
- Hot Tub Folliculitis: Develops from Pseudomonas aeruginosa bacteria found in poorly maintained hot tubs or swimming pools.
- Malassezia Folliculitis: A fungal infection that appears on the chest and back, often mistaken for acne. This type becomes worse with sweating and typically causes intense itching.
- Pseudofolliculitis Barbae: Commonly known as razor bumps, this condition affects people with curly hair, particularly in the beard area after shaving.
- Gram-negative Folliculitis: A rare complication that can develop during long-term antibiotic treatment for acne, causing pustules and cysts.
- Eosinophilic Folliculitis: Primarily affects people with compromised immune systems, causing itchy pustules on the upper body.
- Boils and Carbuncles: These represent severe forms of folliculitis where infection penetrates deeper into the skin, forming painful, pus-filled lumps.
Causes and Risk Factors of folliculitis
The primary causes of folliculitis include:
- Bacterial infections, particularly from Staphylococcus aureus
- Physical damage from tight clothing or sports equipment
- Blocked follicles due to thick moisturisers or tight bandages
- Ingrown hairs resulting from improper shaving techniques
- Excessive sweating creates ideal conditions for infection
Several risk factors increase the likelihood of developing folliculitis. These include:
- Regularly wearing heat-trapping clothing, such as rubber gloves or high boots
- Frequently using poorly maintained hot tubs or public pools
- Diabetes, HIV/AIDS, or other systemic conditions that compromise the immune system
- Long-term use of certain medications, including corticosteroid creams, prednisone, and specific chemotherapy drugs
- Regular shaving, particularly with improper technique, can damage hair follicles and lead to infection
- Participation in activities causing excessive sweating without proper cleaning afterwards
Symptoms of Folliculitis
The condition manifests primarily through visible skin changes and physical discomfort that can affect any area where hair grows.
The most common signs of folliculitis include:
- Red, inflamed bumps that resemble pimples around hair follicles
- White-filled or pus-filled blisters (pustules) that may break open
- Clusters of small bumps appear in groups
- Tender, painful skin in the affected area
- Burning sensation on the skin surface
- Persistent itching that causes discomfort
Complications
Several long-term complications can develop if folliculitis remains untreated:
- Permanent Skin Changes
- Scarring after healing
- Darker or lighter patches of skin (hyperpigmentation or hypopigmentation)
- Permanent hair loss in affected areas
- Progressive Complications
- Recurring infections in the same area
- Spread of infection to other body parts
- Development of larger, painful boils or carbuncles
In rare but serious cases, bacterial folliculitis, particularly those caused by staph infections, can progress to more severe conditions. These may include:
- Cellulitis (deep skin infection)
- Lymphangitis (infection of lymph vessels)
- Blood infections that can affect internal organs
Diagnosis
The diagnostic process usually involves several key steps:
- Physical Examination: Doctors conduct a detailed inspection of the affected areas.
- Medical History Review: Doctors ask about the symptoms and their duration, sweating history, recent hot tub or sauna visit, shaving frequency, and ongoing medications.
- Lifestyle Assessment: Questions about personal habits and activities
- Advanced Diagnostic Methods:
- Skin scraping for microscopic examination
- Bacterial or viral culture swabs
- Skin biopsy in rare cases
Treatments for Folliculitis
For mild cases, several home remedies and self-care measures can effectively manage symptoms:
- Warm Compresses: Apply to affected areas several times daily
- Antibacterial Soap: Use gentle cleansers to keep the area clean
- Loose Clothing: Wear breathable fabrics to reduce irritation
- Over-the-counter Solutions: Apply antibiotic creams or anti-itch lotions
When self-care measures prove insufficient, medical folliculitis treatment becomes necessary. Doctors may prescribe various medications based on the specific type of folliculitis:
- Bacterial Infections:
- Topical antibiotics
- Oral antibiotics for severe cases
- Fungal Folliculitis:
- Antifungal creams or shampoos containing ketoconazole
- Oral antifungal folliculitis medications for persistent cases
- Eosinophilic folliculitis:
- Treatments may include antiretroviral therapy or topical steroids.
- Recurring folliculitis:
- Doctors might recommend long-term preventive measures, including regular use of antibacterial washes or changes in personal care routines.
When to See a Doctor
Immediate Medical guidance is required for the following:
- Folliculitis spreading beyond the original affected area
- Firm or painful spots developing on the skin
- Bumps that are draining fluid
- Fever, chills, or unusual fatigue
- A sudden increase in redness or pain
- A general feeling of being unwell
Prevention
Maintaining proper hygiene forms the foundation of prevention.
- Individuals should wash their skin regularly with mild soap and warm water, particularly after activities that cause sweating.
- Using clean towels and washcloths for each use helps prevent bacterial spread, and these items should be washed in hot, soapy water regularly.
- For those who shave regularly, proper technique is crucial for prevention:
- Use a sharp, clean razor blade for each shaving session
- Apply sufficient shaving cream or gel
- Shave in the direction of hair growth
- Avoid shaving the same area multiple times
- Consider using an electric razor or hair removal alternatives
- Wearing loose-fitting, breathable fabrics helps reduce friction and prevent excessive sweating.
- Only use well-maintained bathtubs & swimming pools & shower immediately after exposure, removing wet swimwear promptly.
Conclusion
Prevention remains the most effective approach to managing folliculitis. Simple daily habits like proper hygiene, wearing loose-fitting clothes, and using clean razors can significantly reduce the risk of developing this condition. People who experience recurring episodes should pay special attention to these preventive measures and consult doctors when symptoms persist or worsen. Regular monitoring and prompt attention to skin changes help maintain healthy skin and prevent complications.
FAQs
1. How do you get rid of folliculitis?
Most cases of folliculitis respond well to proper self-care measures. The most effective treatment approach includes using antibacterial cleansers, applying warm compresses, and keeping the affected area clean. For persistent cases, doctors may recommend:
- Prescription-strength topical antibiotics
- Oral medications for severe infections
- Antifungal treatments for yeast-related cases
- Professional drainage for boils
2. How long can folliculitis last?
Mild cases of folliculitis typically clear up within 7-10 days with proper care. However, some cases may persist for several weeks, particularly if the underlying cause isn't addressed. Chronic folliculitis can last for months if not treated appropriately.
3. Can folliculitis be harmful?
While most cases are mild, untreated folliculitis can lead to serious complications. The infection may spread to deeper skin layers or other body parts. In rare cases, particularly in individuals with weakened immune systems, the infection can enter the bloodstream and cause systemic illness.
4. How to avoid folliculitis?
Prevention focuses on maintaining good hygiene and avoiding irritation. Key preventive measures include wearing loose-fitting clothes, changing out of wet swimwear promptly, and using clean, sharp razors when shaving. Regular cleaning of hot tubs and proper maintenance of pool chemicals also help prevent infection.
5. Is folliculitis serious?
Most cases of folliculitis are mild and resolve without complications. However, the condition requires medical attention if symptoms persist beyond two weeks, spread to new areas, or occur with fever and fatigue. People with compromised immune systems should seek prompt medical care if they develop folliculitis symptoms.
Dr. Shradhha Mahalle

Still Have a Question?