-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Eosinophilia
Symptom, Causes, Diagnosis and Treatment
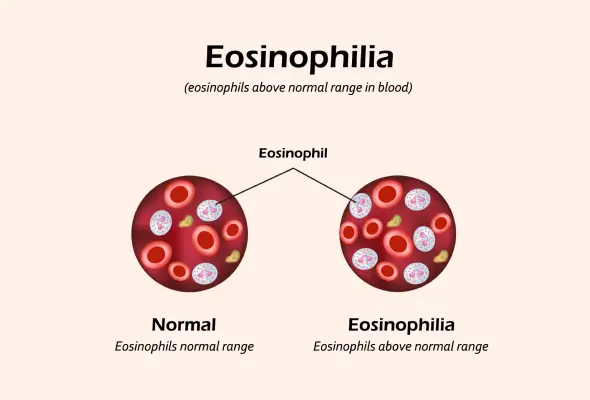
Eosinophilia
Eosinophilia occurs when the body produces an unusually high number of eosinophils in the blood. The condition is diagnosed when there are 500 or more eosinophils per microlitre of blood. Eosinophils, produced in the bone marrow, serve two primary functions in protecting health. First, they defend against allergens and foreign substances entering the body. Subsequently, they protect against fungal and parasitic infections.
The condition can be categorised into two distinct types based on how eosinophils affect the body:
- Blood Eosinophilia: Characterised by elevated levels of eosinophils in the bloodstream
- Tissue Eosinophilia: Marked by increased eosinophil presence in specific body tissues
What are the Symptoms of Eosinophilia?
The severity of eosinophilia disease symptoms varies significantly based on the eosinophil count in the blood and which organs suffer damage. Mild eosinophilia typically presents no noticeable symptoms. Common eosinophilia high symptoms comprise:
- Respiratory Issues:
- Wheezing
- Shortness of breath
- Chronic cough
- Breathing difficulties
- Chest pain
- Constitutional symptoms:
- Low-grade fevers
- Night sweats
- Unexplained fatigue
- Weight loss
- Muscle weakness
- Confusion
- Organ Damage:
- The heart, lungs, spleen, skin, and nervous system face the greatest impact.
- GI Symptoms:
- The Gastrointestinal manifestations often surface through a condition called eosinophilic esophagitis, characterised by vomiting and difficulty swallowing.
- Skin-related Symptoms:
- Skin rashes and persistent itching, particularly in cases linked to cutaneous T-cell lymphoma or eczema.
Causes and Risk Factors of Eosinophilia
Doctors classify eosinophilia into two main categories: primary and secondary eosinophilia. Primary eosinophilia stems from disorders directly affecting blood cell production, whilst secondary eosinophilia develops as a response to other medical conditions.
- Primary Eosinophilia: Several factors contribute to the development of primary eosinophilia:
- Chronic eosinophilic leukaemia
- Myeloid and lymphoid neoplasms with specific gene rearrangements
- Hereditary eosinophilia
- Idiopathic hypereosinophilic syndrome
- Secondary Eosinophilia: Secondary eosinophilia occurs more frequently and has numerous underlying causes:
- Parasitic infections:
- Ancylostomiasis
- Ascariasis
- Cysticercosis
- Schistosomiasis
- Strongyloidiasis
- Fungal and bacterial infections:
- Bronchopulmonary aspergillosis
- Chronic tuberculosis
- Coccidioidomycosis and scarlet fever
- Common allergic triggers:
- Bronchial asthma
- Hay fever
- Reactions to drugs or food.
- Skin conditions:
- Atopic dermatitis
- Eczema
- Pemphigus
- Genetic factors: A single nucleotide polymorphism in the gene coding thymic stromal lymphopoietin is located on the pseudoautosomal region of the X and Y chromosomes.
Risk factors associated with specific types of eosinophilia include:
- Male gender
- Caucasian race
- History of atopy
- Family history
- Environmental elements, particularly the timing and nature of food exposure to the developing immune system
- Autoimmune diseases, including inflammatory bowel disease, autoimmune myocarditis, vasculitis, and sarcoidosis,
- Certain medications like interleukin-1 and interleukin-6 inhibitors
Complications of Eosinophilia
Persistent high levels of eosinophils can lead to serious complications affecting multiple organs throughout the body.
- Organ damage occurs through several mechanisms:
- Tissue infiltration
- Formation of fibrosis
- Development of thrombosis
- Allergic inflammation
- Cardiac Complications: The heart faces particular risks from eosinophilia. A condition called Löffler endocarditis can develop, potentially causing:
- Blood clot formation
- Heart failure
- Heart attacks
- Valve dysfunction
- Respiratory System: Inflammation can cause lung damage and respiratory failure
- Nervous System: May lead to confusion and encephalopathy
- Skin: Can result in rashes and inflammation
- Gastrointestinal Tract: Affects the oesophagus, stomach, and intestines
Diagnosis of Eosinophilia
The initial diagnostic tool is a complete blood count (CBC) with a differential white blood cell count.
Blood eosinophilia receives confirmation upon detecting more than 500 eosinophils per cubic millimetre of blood. Doctors categorise the severity into three distinct levels:
- Mild: 500-1,500 cells/mm³
- Moderate: 1,500-5,000 cells/mm³
- Severe: Above 5,000 cells/mm³
Given the diverse manifestations of eosinophilia, doctors conduct thorough physical examinations focusing on the following:
- Heart assessment
- Skin examination
- Neurological evaluation
- Pulmonary system check
Based on clinical findings, doctors might recommend additional diagnostic tests:
- Stool examination: Identifies parasitic infections
- Chest X-rays: Detects lung infections, inflammation, or conditions like eosinophilic pneumonia
- Urinalysis: Helps assess kidney involvement or urinary tract infections
- Liver function tests: Evaluate liver health
- Kidney function assessment: Checks for renal diseases that may contribute to elevated eosinophils
- Cytogenetic testing: Identifies chromosomal abnormalities associated with hematologic disorders
- FISH analysis: Detects specific genetic mutations linked to eosinophilic syndromes or cancers
- Skin biopsies to identify conditions like pemphigoid, eczema, or mycosis fungoides
- Ultrasound examination: Helps detect organ (liver, spleen, or lymph node) abnormalities linked to eosinophilia-related conditions
- Echocardiography: Assesses heart function and detects eosinophilic myocarditis
- Serum troponin levels: Measures heart muscle damage, which can occur in eosinophilic myocarditis
- Pulmonary function tests
- Evaluate lung function and detect respiratory conditions
Treatment
For mild cases, doctors recommend constant monitoring through recurring laboratory tests to track eosinophil levels.
- In instances where medications trigger eosinophilia, doctors typically advise discontinuing or modifying the problematic drug.
- Corticosteroids remain the most effective therapy for reducing eosinophil counts in both blood and tissue. Proton pump inhibitors for acid-associated oesophagitis
- Fluticasone inhalers for controlling inflammation
- Budesonide liquid mixed with specific agents
- Biologics for various eosinophilic conditions
- Doctors often prescribe treatments for allergic reactions to control the body's immune response.
- In cases involving parasitic or fungal infections, doctors carefully avoid steroid treatments, as these medications might worsen the condition.
- Several lifestyle modifications support treatment effectiveness:
- Maintaining a balanced diet free of acidic foods
- Reducing stress levels through relaxation techniques
- Keeping living spaces clean to minimise allergen exposure
- Increasing vitamin D consumption
- Incorporating anti-inflammatory foods like ginger and turmeric
- Doctors often recommend the six-food elimination diet for patients with eosinophilic disorders affecting the digestive system. This dietary approach excludes common trigger foods, including eggs, soy, nuts, fish, milk, shellfish, and wheat.
- For severe cases unresponsive to standard treatments, doctors might consider nonmyeloablative allogeneic hematopoietic stem cell transplantation, though its role remains under investigation.
When to See a Doctor
Certain symptoms of eosinophilia warrant immediate medical attention, primarily those affecting vital organs:
- Respiratory System Signs:
- Persistent wheezing
- Severe shortness of breath
- Difficulty breathing
- Cardiovascular Indicators:
- Chest pain
- Symptoms of heart failure
- Unexplained fatigue
- Gastrointestinal Issues:
- Throat discomfort
- Stomach pain
- Difficulty swallowing
Preventions of Eosinophilia
Since allergies rank as the most common trigger for elevated eosinophil levels, controlling allergic reactions stands as the first line of defense.
- Maintaining a Clean Environment: Creating a dust-free living space plays a vital role in prevention. Regular cleaning routines help minimise exposure to common allergens. Essential practices include:
- Dusting at least once weekly to prevent dust mite accumulation
- Keeping windows closed during peak pollen seasons
- Maintaining proper ventilation
- Following strict personal hygiene protocols
- Dietary Considerations: Food choices significantly influence eosinophil levels. A comprehensive approach to dietary management includes:
- Thoroughly washing fruits and vegetables
- Avoiding uncooked meats, fish, and shellfish
- Steering clear of freshwater prawns, snails, and slugs
- Consuming only boiled liquids
- Lifestyle Modifications: Several lifestyle changes can effectively reduce the risk of developing eosinophilia:
- Quitting smoking
- Limiting alcohol consumption
- Following a balanced diet low in acidic foods
- Maintaining a healthy weight
- For individuals with acid reflux-related eosinophilia, dietary adjustments prove beneficial. Recommended foods include lean meats, whole grains, and fresh produce. Conversely, certain items warrant avoidance:
- Fried foods
- Tomatoes
- Chocolate
- Mint
- Garlic
- Onions
- Coffee
- Medication Management: Careful attention to medication use helps prevent drug-induced eosinophilia. Certain medications associated with increased eosinophil counts include:
- Amphetamines
- Interferon
- Some antibiotics
- Psyllium-containing laxatives
- Tranquillisers
Conclusion
Understanding eosinophilia remains crucial for effective management of this condition. Though mild cases might show no symptoms, elevated eosinophil counts can lead to serious organ damage when left untreated. Doctors typically recommend lifestyle changes, medication adjustments, or specific treatments based on individual cases. Additionally, preventive measures like maintaining a clean environment and following proper dietary guidelines help reduce the risk of developing eosinophilia.
FAQs
1. Is eosinophilia serious?
High eosinophil counts can indicate both mild and serious conditions. Without treatment, hypereosinophilic syndrome can worse. With proper medical intervention,it can be treated.
2. What can happen if eosinophil counts are high?
Elevated eosinophil levels can damage multiple organs through inflammation. The heart faces particular risks, potentially developing Löffler endocarditis, which leads to blood clots, heart failure, and valve problems. Other complications affect the lungs, skin, and nervous system.
3. What causes an increase in eosinophils?
Several factors trigger elevated eosinophil counts. Common causes include allergic reactions, parasitic infections, and certain medications. In some cases, blood disorders, autoimmune conditions, or specific genetic changes might raise eosinophil levels.
4. Which food is not good for eosinophilia?
People with eosinophilia should avoid:
- Acidic foods
- Fried items
- Tomatoes
- Chocolate
- Garlic and onions
- Coffee
5. Which food reduces eosinophils?
Beneficial foods for managing eosinophil levels include:
- Fresh fruits and vegetables
- Lean meats
- Whole grains
- Foods rich in vitamin D
- Natural anti-inflammatories like honey, turmeric, and ginger
6. Can eosinophilia be cured?
Eosinophilia remains a chronic condition without a definitive cure.
7. Can eosinophils go back to normal?
Eosinophil levels often return to normal after treating the underlying condition. Furthermore, anti-inflammatory medications alongside lifestyle changes help maintain healthy eosinophil counts. Regular monitoring through blood tests ensures levels stay within normal ranges.
Still Have a Question?


