-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Endometriosis
Symptom, Causes, Diagnosis and Treatment
Endometriosis
Endometriosis is a condition that remains shrouded in mystery and misunderstanding despite affecting millions of women worldwide. The importance of knowing this condition cannot be neglected, as it plays a pivotal role in the health and well-being of countless individuals. By shedding light on what endometriosis is, its symptoms, and its impacts, we can pave the way toward more effective treatments and, ultimately, a better quality of life for those affected.
What is Endometriosis?
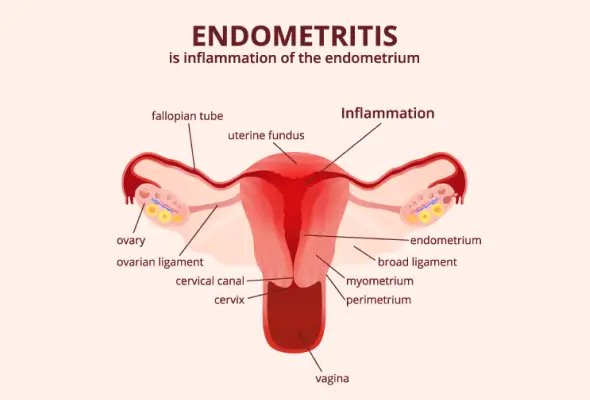
Endometriosis is a chronic gynaecological condition. In endometriosis, tissue identical to the lining of the uterus (endometrium) grows outside the uterus. The misplaced endometrial tissue can be found on the woman's ovaries, fallopian tubes, other organs, and, in rare cases, even outside the abdomen.
Endometriosis Symptoms
Common symptoms of endometriosis include:
- Pelvic pain, especially during menstrual periods
- Heavy or irregular bleeding
- Severe abdominal cramps during menstrual cycles
- Painful intercourse
- Infertility or difficulty getting pregnant
- Fatigue, nausea, and digestive issues
Endometriosis Stages
This condition is classified into four stages based on the size, location, and depth of the endometrial tissue implants. Most doctors use the American Society of Reproductive Medicine (ASRM) scale to determine the stage:
- Stage I: Minimal Endometriosis with a few small implants, wounds, or lesions and no or little scar tissue
- Stage II: Mild Endometriosis with more, deeper implants and some scar tissue
- Stage III: Moderate Endometriosis with many deep implants, small cysts may be present on one or both ovaries and thick bands of scar tissue.
- Stage IV: Severe Endometriosis with widespread deep implants, thick adhesions, and large cysts may be present on one or both ovaries.
What Causes Endometriosis?
The exact reason for endometriosis is still unknown. However, researchers have studied several potential factors that may contribute to its development:
- Retrograde Menstrual Flow: During menstruation, some of the tissue shed from the uterine lining may flow backwards through the fallopian tubes, reaching the pelvic cavity. These endometrial cells can then implant and grow on the ovaries or fallopian tubes in the pelvic region.
- Genetic Factors: Endometriosis tends to run from one generation to another.
- Immune System Dysfunction: A faulty immune system may fail to recognise and destroy endometrial tissue growing outside the uterus.
- Hormonal Imbalances: The hormone estrogen appears to promote the endometrial tissue growth, both inside and outside the uterus.
- Surgical Complications: Endometrial tissue may be inadvertently moved or implanted in other body areas during abdominal or pelvic surgeries, such as a Cesarean section or hysterectomy.
- Other Potential Factors:
- Menstrual cycles occurring more frequently than every twenty-eight days
- Menstrual periods with heavy bleeding lasting longer than seven days
- Low body mass index
- Structural issues with the vagina, cervix, or uterus that prevent proper menstrual flow
- Starting menstruation at an early age
- Starting menopause at an older age
Endometriosis Diagnosis
Doctors evaluate symptoms and identify the presence and extent of endometriosis, including:
- Pelvic Examination: Your doctor feels areas in your pelvis with one or two gloved fingers to check for unusual changes, painful spots, or irregular growths.
- Ultrasound: It can help detect cysts associated with endometriosis, called endometriomas.
- Magnetic Resonance Imaging (MRI): MRI can provide valuable information about the location and size of endometriosis growths.
- Laparoscopy: Your doctor will perform a laparoscopy only after learning your full medical history and a complete physical and pelvic examination.
Endometriosis Treatment
The treatment of endometriosis often involves a combination of approaches, including medication and surgery.
- Pain Management: For managing endometriosis-related pain, doctors may recommend:
- Non-steroidal Anti-inflammatory Drugs (NSAIDs) to help alleviate painful menstrual cramps
- Muscle Relaxants to decrease cramping and pain in the pelvic and bladder muscles. Antidepressants can be beneficial for individuals with chronic pain, including nerve irritation from endometriosis.
- Anti-convulsant Medications can help women manage endometriosis-related pain.
- Hormone Therapy:
- Hormonal treatments aim to slow the growth of endometrial tissue and prevent new tissue from forming. However, they are not suitable for women trying to conceive.
- Surgery: Doctors may recommend surgical interventions when medical treatment fails to provide relief.
- Conservative Surgery: This approach involves the removal of tissue of endometriosis while preserving the uterus and ovaries, potentially improving fertility and reducing pain.
- Hysterectomy: In severe cases, a hysterectomy (removal of the uterus) with or without ovary removal may be considered as a last resort when other treatments have not worked.
- Interventional Therapies:
- Nerve Blockade: This diagnostic and therapeutic procedure involves injecting anaesthetics near specific nerves to relieve temporary pain.
- Muscle Injections: Endometriosis can cause muscle spasms and trigger points, which can be treated with local anaesthetic or corticosteroid injections.
- Complementary Therapies:
- Some women find relief through complementary therapies like physical therapy, behavioural therapy, and acupuncture.
Complications
Endometriosis can lead to various complications if left untreated. Some of the potential complications include:
- Fertility problems or difficulty getting pregnant
- Adhesions of endometriosis tissue with organs
- Ovarian cysts, known as endometriomas, can form. These fluid-filled cysts in the ovaries can sometimes become large and painful, especially if the endometriosis tissue is on or near the ovaries
- Endometriosis raises the risk of ovarian cancer
- Bladder and bowel complications
- Individuals with endometriosis may experience fatigue, constipation, bloating, or nausea, especially during menstrual periods
- Additionally, the chronic pain and challenges associated with endometriosis can lead to mental health issues like depression and anxiety
When to See a Doctor
Consult your doctor if you notice any of the following:
- Excruciating menstrual cramps that disrupt your daily activities or do not respond to over-the-counter pain medication
- Chronic pelvic pain that occurs before, during, or after your menstrual period or pain that radiates to your back, legs, vagina, or rectum
- Excessively heavy or prolonged menstrual bleeding or bleeding between periods
- Pain during sexual intercourse, bowel movements, or urination
Prevention
While there is no definitive way to prevent endometriosis, certain lifestyle modifications may help reduce the risk or manage symptoms if you have the condition.
- Regular Exercise: Exercise helps maintain an optimal body weight and lower body fat percentage, decreasing the amount of estrogen circulating. A lower estrogen level may slow the progression of endometriosis.
- Limit Alcohol Consumption: Consuming large amounts of alcohol can raise estrogen levels in the body.
- Moderate Caffeine Intake: Limit your caffeine intake or opt for decaffeinated beverages.
Conclusion
Endometriosis is a chronic condition affecting many women worldwide. Recognising early signs and consulting doctors sets the stage for managing the condition effectively, potentially mitigating the long-term impacts on fertility and overall well-being. The discourse on endometriosis treatment underscores the necessity of a tailored approach, factoring in individual symptoms and treatment responses, to optimise outcomes.
FAQs
1. Is endometriosis genetic?
Endometriosis seems to have a genetic component. Research has shown that women with a first-degree relative (mother, sister, or daughter) affected by endometriosis have a higher risk of getting the condition themselves.
2. What happens if endometriosis is left untreated?
If left untreated, endometriosis can worsen over time, leading to several potential complications:
- Severe pain
- Damage to reproductive organs, fallopian tubes, and ovaries
- Complications like urinary incontinence and bowel obstruction
- Heightened risk of developing certain chronic diseases and chronic pain conditions.
3. Can endometriosis go away on its own?
Endometriosis can sometimes go into remission or even disappear, but this is not a common occurrence. While symptoms may improve temporarily, especially during pregnancy or menopause, the condition often requires medical treatment to manage pain and complications.
4. At what age does endometriosis start?
Endometriosis typically develops during the reproductive years, which is the period between the onset of menstruation (menarche) and menopause. It is most commonly diagnosed in women between the ages of 25 and 40.
5. Is endometriosis very serious?
Yes, endometriosis is considered a serious condition that can significantly impact a woman's quality of life and overall well-being. While not life-threatening, endometriosis can be debilitating and have far-reaching consequences if left untreated. It can cause severe endometriosis pain, chronic pelvic discomfort, infertility, organ damage, & an increased risk of certain cancers.
To Book an Appointment, call:
Still Have a Question?




