-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Endocarditis
Symptom, Causes, Diagnosis and Treatment
Endocarditis
Endocarditis, a serious condition affecting the inner lining of the heart chambers and valves, often starts with something as simple as poor dental hygiene. This infection can result in severe damage to the heart if left untreated, making it crucial to understand its symptoms, reasons, and treatment options.
This article aims to provide essential information about endocarditis, covering its various types, signs and symptoms, and potential causes. We'll explore the risk factors that make some people more vulnerable to this condition and discuss the complications that can arise if it's not addressed promptly.
What is Endocarditis?
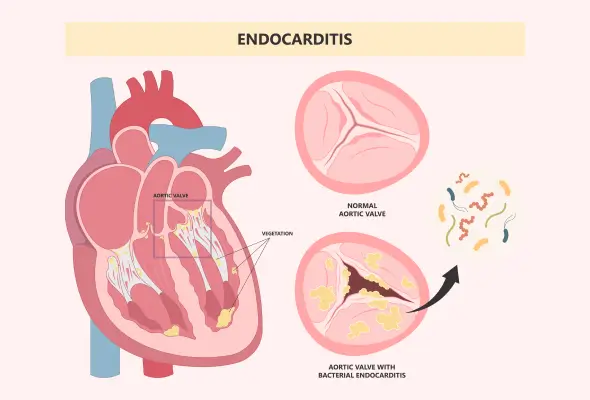
Endocarditis is a serious and potentially life-threatening inflammation of the innermost lining of the heart chambers (atria and ventricles) and valves, known as the endocardium. This condition usually occurs when bacteria (rarely fungi) enter the blood circulation and attach to damaged areas in the heart. The infection can affect the heart muscle, valves, or lining, leading to severe complications if left untreated.
There are three main endocarditis types:
- Acute Endocarditis: This acute condition develops suddenly and rapidly damages the heart's structures and can become life-threatening within days.
- Subacute Endocarditis: This endocarditis progresses slowly over weeks or months. Subacute endocarditis develops from a particular group of streptococci bacteria usually present in your mouth and throat.
- Prosthetic Valvular Endocarditis: This type of endocarditis affects people who have had heart valve replacement surgery within the past year.
Causes of Endocarditis
Bacterial infections primarily cause endocarditis, though fungi can also be responsible in rare cases. The infection occurs when harmful microorganisms enter the blood flow and attach to damaged areas of the heart, particularly the valves. Common activities that can lead to bacteria entering the blood include dental procedures, eating, brushing teeth, and even using the toilet.
During the infection, the endocardium, clumps of bacteria or fungi, and other components are formed, known as vegetations. These vegetations can break away from the endocardium and spread to other body parts, resulting in various cardiac conditions.
Symptoms of Endocarditis
Endocarditis symptoms can differ from person to person and may develop slowly or suddenly, depending on the type of germs causing the infection and existing heart problems. Common endocarditis signs and symptoms include:
- Fever above 38.4°C
- Night sweats
- Fatigue
- A moderately fast heart rate
- Chest pain when breathing
- Shortness of breath
- A new or changed heart murmur
- Aching joints and muscles
- Swelling in the feet, legs, or belly
Less common symptoms include:
- Unexplained weight loss
- Blood in the urine
- Tenderness under the left rib cage
- Red, purple, or brown spots on the soles of their feet or palms (known as Janeway lesions)
If you experience any of these endocarditis symptoms, especially if you have a history of heart problems, it's crucial to see a doctor promptly for proper evaluation and diagnosis.
Risk Factors
Several factors increase the likelihood of developing endocarditis, including:
- Older people, especially those over 60, are at higher risk.
- People with artificial heart valves or damaged heart valves due to conditions like rheumatic fever are more susceptible.
- Congenital heart defects and implanted heart devices also raise the risk.
- Intravenous drug use with contaminated needles is a significant concern.
- Poor dental health can allow bacteria to enter the bloodstream through gum cuts.
- Long-term catheter use increases the risk as well.
- Men are twice as likely to develop endocarditis compared to women.
- Other endocarditis risk factors include a history of endocarditis, a suppressed immune system, and certain heart conditions like hypertrophic cardiomyopathy.
It's important to note that endocarditis rarely occurs in people with healthy hearts.
Complications of Endocarditis
Endocarditis can lead to severe complications affecting various organs, such as:
- Heart failure is a common issue, often resulting from valve damage. Vegetations can break loose, causing problems in other body parts. These may lead to stroke, kidney damage, or lung abscesses.
- Blood clots can form, potentially causing a pulmonary embolism.
- In some cases, pockets of pus (abscesses) may develop in the heart, brain, or other organs.
- Neurological complications, like ischemic stroke or intracranial hemorrhage, affect 15% to 30% of cases.
- Acute renal failure and splenic infarcts are also possible.
These complications can occur simultaneously, making endocarditis a potentially life-threatening condition that needs prompt medical attention.
Diagnosis of Endocarditis
Diagnosing endocarditis involves a comprehensive approach:
- Medical History: Doctors will inquire about your symptoms, how they started, recent dental or surgical procedures, intravenous drug use, and whether you have any risk factors for endocarditis.
- Physical Evaluation: Doctors will listen to your heart for abnormal sounds (heart murmur) and check for other signs of infection, such as small red spots on the skin and swelling in the feet or ankles.
- Blood Cultures: These tests are crucial for identifying the causative microorganism and guiding treatment.
- Complete Blood Count (CBC): To check for elevated white blood cell count, indicating infection.
- Erythrocyte Sedimentation Rate (ESR) and C-reactive Protein (CRP) Assessment: To detect inflammation in the body.
- Echocardiography: Echocardiography plays a vital role in diagnosis, with transoesophageal echocardiography (TEE) being more sensitive than transthoracic echocardiography (TTE) for detecting veget ation and other cardiac abnormalities associated with endocarditis.
- Electrocardiogram (ECG): ECG monitors the heart's electrical activity and detects any abnormalities caused by endocarditis.
In cases of culture-negative endocarditis, doctors may perform specialised serological tests or molecular methods to identify fastidious organisms.
Endocarditis Treatment
Treatment for endocarditis typically involves:
- Antibiotics: Patients usually receive intravenous antibiotics for several weeks, but after completing a course of IV treatment, they may also need to take oral antibiotics. Antibiotics are typically given for two to six weeks to eliminate the infection completely. The choice of antibiotics generally depends on the specific bacteria causing the infection. For prosthetic valve endocarditis, treatment is often more complex and may require a longer course of antibiotics.
- Antifungal Medications: Doctors prescribe antifungal medicines to treat endocarditis caused by a fungal infection.
- Surgery: In some instances, doctors may perform surgery to repair or replace damaged heart valves.
When to See a Doctor
If you experience symptoms of endocarditis, it's crucial to seek medical guidance promptly, especially if you have a history of heart conditions. Don't wait for symptoms to worsen before consulting a doctor. Even if you're unsure whether your symptoms indicate endocarditis, it's better to err on the side of caution. Contact your doctor if you have signs and symptoms of infection, such as fever, chills, or joint pain. It's important to note that while colds and flu don't cause endocarditis, they may have similar symptoms.
If you've been diagnosed with endocarditis and notice worsening symptoms like shortness of breath or headaches, inform your doctor immediately. Call emergency services without delay in case of sudden, severe symptoms that might indicate a stroke.
Preventions
Preventing endocarditis involves several key steps:
- Maintaining good oral hygiene is crucial. Brush your teeth twice daily, regularly floss, and have dental check-ups every six months.
- If you're at high risk of endocarditis, inform your dentist and doctor. They may recommend antibiotics before certain dental procedures.
- Avoid illegal drug use, especially intravenous drugs, as they significantly increase the risk.
- Know the signs and symptoms of endocarditis and seek medical intervention promptly if you develop any.
- For those with congenital heart defects, follow your doctor's advice on preventive measures.
Conclusion
Endocarditis is a serious heart infection that can have severe consequences if not treated promptly. Understanding its signs and symptoms and knowing when to seek medical help can significantly affect the outcome of this potentially life-threatening condition. Maintaining good oral hygiene and following your doctor's advice are crucial steps to prevent endocarditis, especially for high-risk patients. Remember, while this infection is rare in healthy hearts, it's essential to be aware of the risks and take necessary precautions. By staying informed and vigilant, you can protect your heart health and ensure a swift response if any concerning symptoms arise.
FAQ's
1. Can you recover from endocarditis?
Recovery from endocarditis is possible with prompt and appropriate treatment. Many patients successfully recover with antibiotic therapy, which may last several weeks. However, the recovery process can be lengthy, and long-term follow-up care is often required to prevent recurrence.
2. What are the warning signs of endocarditis?
Warning signs of endocarditis include fever, chills, night sweats, fatigue, and unexplained weight loss. Other symptoms may involve chest pain, shortness of breath, and a new or changed heart murmur. Some patients might experience aching joints and muscles, swelling in the feet or legs, and skin changes such as red or purple spots on the palms or soles.
3. What are the three stages of endocarditis?
Endocarditis develops in three stages:
Bacteremia: Microorganisms enter the bloodstream.
Adhesion: The microorganisms attach to damaged areas of the heart's inner lining.
Colonisation: The organisms multiply, forming vegetation and causing inflammation.
4. Who is at risk for bacterial endocarditis?
People at higher risk for bacterial endocarditis include those with artificial heart valves, damaged heart valves, or congenital heart defects. Other risk factors involve a history of endocarditis, intravenous drug use, poor dental hygiene, having long-term catheters and having weakened immune systems.
5. Is endocarditis permanent?
Endocarditis itself is not permanent if treated promptly and effectively. However, it can cause permanent damage to heart valves or other complications if left untreated or if treatment is delayed. Some patients may experience long-term effects or require ongoing medical care, especially if they have pre-existing heart conditions or the infection has caused significant damage.
6. Is endocarditis treatable?
Endocarditis is treatable, primarily with high doses of intravenous antibiotics. Treatment typically lasts for several weeks and may require hospitalisation initially. In some cases, antifungal medications are used if fungi cause the infection. Doctors may perform surgery to repair or replace damaged heart valves or to remove infected tissue.
Still Have a Question?