-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Dislocation
Symptom, Causes, Diagnosis and Treatment
Dislocation
Dislocation is an excruciating injury that occurs when bones in a joint are driven out of their normal position. Understanding the types of dislocations, their causes, and available treatments is crucial for proper care and recovery. This article explores the symptoms of dislocation, potential complications, and methods for diagnosis. It also discusses dislocation treatment options, prevention strategies, and when to seek medical help. By learning about dislocation, individuals can better protect themselves and know how to respond if this injury occurs.
What is a Dislocation?
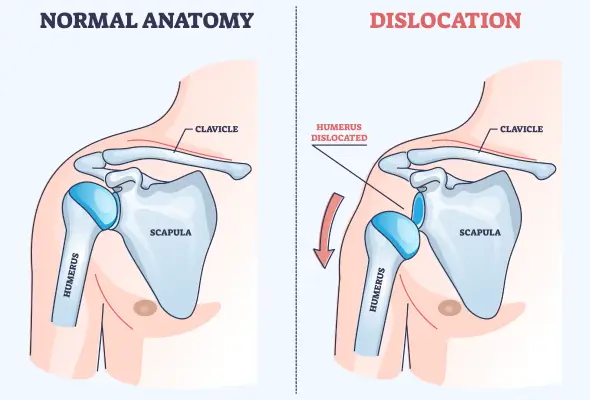
A dislocation is a joint injury. It occurs when the ends of two or more connected bones come apart completely. It happens when extreme force is put on a ligament, causing the bones in a joint to be forced out of their normal position. This injury can be painful and temporarily deform and immobilise the joint. Joints are places where two bones meet in the body, allowing movement and providing support from head to toe.
Dislocations can happen to any joint in the body, but some are more common than others. The shoulder is the most frequently dislocated joint, followed by fingers, patella (kneecap), elbow, and hip.
Types of Dislocation
Dislocations can occur in multiple joints throughout the body, each with its own unique characteristics and challenges, such as:
- Shoulder Dislocations: They happen when the humerus (upper arm bone) thrusts out of the shoulder socket, especially due to a fall or during contact sports.
- Finger Dislocations: They often affect the middle knuckle
- Wrist Dislocations: Also called hand joint dislocation, wrist dislocation can involve any of the eight small wrist bones.
- Elbow Dislocations: They require significant force and often involve associated fractures. These dislocations can trap nerves and blood vessels, necessitating urgent medical attention.
- Kneecap (Patellar) Dislocations: Patellar dislocations are common in teenagers, especially girls. The kneecap moves sideways out of its groove, causing pain and difficulty in knee movement.
- Hip Dislocations: They result from major injuries like road accidents and can lead to significant complications. Most hip dislocations occur backwards, causing the affected leg to turn inwards.
- Ankle and Foot Dislocations: Though less common, these can occur in severe accidents or sports injuries.
Dislocations can be classified into the following two types based on how far the bones in the joints were shifted:
- Complete Dislocation: A complete dislocation (luxation) occurs when the bones in the joint are entirely separated and pushed out of the joint place.
- Partial Dislocation: A partial dislocation (subluxation) occurs when a bone is partially pulled or pushed out of a joint place.

Causes and Risk Factors of Dislocation
Dislocation can happen due to various reasons, with some joints being more susceptible than others. Here are some common causes of dislocation:
- Falls: Falling is the most common cause of dislocation. The force transmitted to the joint when the body hits the ground, often combined with a turning motion, can rotate the joint out of its socket.
- Sports-related Activities: Contact sports like football and hockey pose a higher risk, especially for shoulder dislocations. Other sports that involve potential falls, such as downhill skiing, gymnastics, and volleyball, can also result in dislocation.
- Accidents: Motor vehicle accidents (cars or bikes) are a leading cause of dislocations.
Certain factors increase the risk of experiencing a dislocation. These include:
- Being male between adolescence and 30 years of age OR a woman aged 61-80 years for shoulder dislocations.
- Having a prior history of joint instability or conditions like Ehlers-Danlos syndrome, which weakens connective tissues, also raises the risk.
Symptoms of Dislocation
Dislocation profoundly impacts the affected joint, causing a range of noticeable symptoms. These include:
- Intense pain in the injured area
- Swelling
- Bruising around the joint
- A visibly deformed or out-of-place joint
- Affected areas may feel tender to the touch
- Inability to move or use the dislocated joint
- Numbness, weakness, or tingling sensations near the injury site
- Muscle spasms in the affected area
- Sciatic Nerve Injury (with hip dislocations)
Complications
Dislocation can lead to several significant complications if left untreated or improperly managed. These may include:
- Increased risk of future dislocations
- Fractures in the bones surrounding the joint
- Damage to the surrounding soft tissues, including ligaments, nerves, and blood vessels, can result in long-term instability, weakness, or numbness in the affected area.
- Severe dislocations can disrupt blood flow to the limb. This can lead to tissue death (necrosis) if not addressed promptly.
- Infections are a rare but serious complication, particularly if the skin is broken during the dislocation. These infections can spread to the bone, causing osteomyelitis, which is challenging to treat.
Diagnosis
The doctor first assesses the affected joint and surrounding area. Patients are asked about their symptoms and the circumstances leading to the injury. They may conduct several tests, including:
- X-rays: An X-ray of the joint is usually the first imaging test ordered to confirm a dislocation and detect any associated fractures.
- Magnetic Resonance Imaging (MRI) scans: MRIS can reveal damage to surrounding soft tissues like ligaments and tendons. This is especially helpful for shoulder and knee dislocations, where labral tears or rotator cuff injuries might occur.
- Computed Tomography (CT) Scans: These provide detailed images of bones and can be helpful in complex dislocations, particularly in the elbow or hip.
- Ultrasound: It allows real-time evaluation of soft tissues and can help assess rotator cuff injuries.
Treatment for Dislocation
Treating a dislocation is all about putting the joint back into its correct position, a process known as relocation or closed reduction. An expert should only perform this procedure, as attempting to reposition the joint on your own can lead to serious complications.
Following relocation, treatment often involves immobilisation using a splint, sling, or brace to hold the joint in place while it heals.
Rest is crucial during this period to avoid stress on the affected joint.
In some cases, particularly for severe dislocations or those with associated injuries, surgery may be necessary. This could involve repairing damaged soft tissues or resetting the joint if closed reduction is unsuccessful.
When to See a Doctor
Seeking medical attention promptly is crucial when dealing with a suspected dislocation. It's essential not to attempt to push the joint back into place by yourself or allow anyone who isn't a trained doctor to move or touch the injured joint.
Go for immediate emergency medical help if you experience:
- Chest pain
- Difficulty breathing
- Weakness or numbness on one side
- Slurred speech
- Fainting
- Changes in mental state
Prevention
While not all dislocations can be prevented, you can take several precautionary measures to reduce your risk. These include:
- Wear appropriate protective equipment during sports or physical activities and avoid playing through pain.
- Give your body time to rest and recover after intense activity.
- Always warm up before exercising and cool down afterwards.
- To prevent falls, keep your home and workspace clutter-free.
- Use proper tools or equipment to reach high places, never standing on chairs or countertops.
- If you have difficulty walking or an increased risk of falls, consider using a walker or cane.
- Maintaining a healthy body weight is necessary, as excess body weight can cause undue stress on joints, particularly the hip.
- Practise good posture to reduce strain on the joints & consider working with a physical therapist to develop a posture-improvement plan.
- Strengthening exercises targeting specific muscle groups can help support joints and reduce the risk of dislocation.
- Include exercises like hip extensions and abductions in your routine, but consult a fitness professional to create a safe workout plan.
- Wearing protective gear such as hip pads can help absorb impact and protect joints from injury for those participating in contact sports.
- Consider low-impact activities like cycling or swimming if you have a history of joint problems.
Conclusion
Prompt medical attention is key when dealing with a suspected dislocation. Proper diagnosis and treatment, including closed reduction and rehabilitation, are essential to restore joint function and prevent future complications. You can better protect your joints and maintain overall musculoskeletal health by staying informed and taking preventive measures.
FAQs
1. What do dislocations cause?
Dislocations cause intense pain, swelling, and an inability to use the affected joint normally. In some cases, dislocations can lead to numbness or abnormal sensations in the affected limb.
2. Is dislocation painful?
Yes, dislocation is typically very painful. The pain is usually immediate and severe, especially when attempting to move or put weight on the injured part.
3. What is the first aid for dislocation?
First aid for dislocation involves immobilising the affected limb to prevent further injury. Support the injured area with a makeshift splint, sling, or pillow. Elevate the limb if possible to reduce swelling. Apply ice wrapped in a towel to relieve pain and control swelling, and immediately contact your doctor.
4. Can you reduce a dislocation?
Reducing a dislocation should only be done by trained doctors. Attempting to relocate a dislocated joint yourself can cause further damage to surrounding tissues, nerves, and blood vessels.
5. What is the recovery time for a dislocation?
Recovery time for a dislocation varies and depends on the joint affected and the severity of the injury. Generally, a dislocated joint takes about 6 to 8 weeks to heal fully.
6. What to do immediately after dislocation?
Immediately after a dislocation, seek emergency medical care. While waiting for help, keep the affected joint still and supported. Apply ice to reduce pain and swelling. Do not attempt to move the joint back into place yourself.
Dr. Anurag Kawle

Still Have a Question?



