-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Croup Cough
Symptom, Causes, Diagnosis and Treatment
Croup Cough
Have you ever heard a child's cough that sounds like a barking seal? This distinctive sound often indicates croup, a common childhood illness that affects the upper airways. Croup cough can cause worry for parents, but understanding its symptoms and treatment approaches can help manage the condition effectively.
While croup cough can be distressing, it's usually treatable at home. However, in some cases, medical attention may be necessary. This blog will explore the causes, signs, and treatment of croup, providing parents with the knowledge to identify and address this condition confidently.
What is Croup?
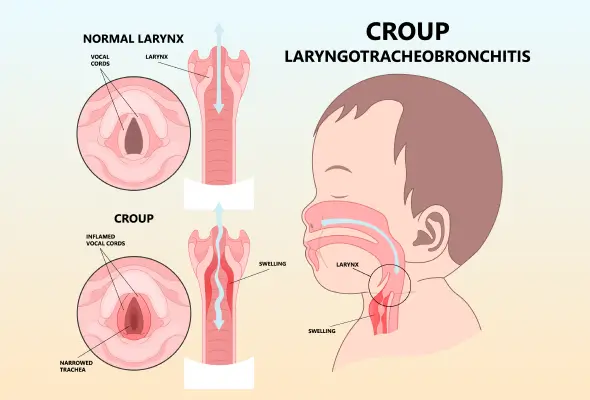
Croup, or laryngotracheobronchitis, is a respiratory infection primarily affecting young children. This condition causes swelling in the voice box (larynx) and windpipe (trachea), narrowing the airway below the vocal cords. As a result, children with croup experience difficulty breathing and a harsh, raspy sound when inhaling. The condition is typically caused by viral infections, with the swelling and irritation extending to the bronchial tubes (bronchi) as well.
The hallmark of croup is a distinctive cough that sounds remarkably similar to a barking seal. This unique sound occurs when air is forced through the narrowed passageway, causing the swollen vocal cords to vibrate. Additionally, children with croup often exhibit a high-pitched whistling sound called stridor when they breathe in.
Symptoms of Croup
Croup typically starts with symptoms resembling a common cold. The condition can worsen over the next 12 to 48 hours, and the characteristic barking cough may begin and often worsen at night.
May notice their child experiencing:
- Hoarseness
- Fever
- Noisy or laboured breathing
- A harsh, raspy sound when inhaling (stridor)
- Rash
- Eye redness (conjunctivitis)
- Swollen lymph nodes
In moderate to severe cases, children might show:
- Difficulty breathing
- Restlessness or nervousness
- Retractions (sucking in of the skin around the ribs and top of the breastbone)
- Cyanosis (blue-tinged skin)
- Crying, coughing, and distress can exacerbate symptoms, creating a cycle of worsening conditions.
While croup usually lasts 3 to 5 days, monitoring symptoms closely is essential.
Causes of Croup
Croup primarily stems from viral infections. The most common culprit is the parainfluenza virus, but other viruses like influenza, respiratory syncytial virus (RSV), measles, and adenovirus can also cause croup. These viruses lead to swelling in the upper airways, making breathing difficult for children.
Children typically contract these viruses by inhaling infected respiratory droplets that have been coughed or sneezed into the air. Additionally, virus particles can survive on surfaces such as toys. An infection may follow if a child touches these contaminated surfaces and then touches their nose, eyes, or mouth.
In rare cases, bacteria can complicate the viral infection, exacerbating breathing difficulties. However, bacterial causes of croup are much less common than viral ones.
Diagnosis of Croup
Doctors typically diagnose croup based on the child's symptoms and a physical examination. The most common signs are a distinctive barking cough and stridor and a high-pitched whistling sound when breathing in. These symptoms often allow parents to identify croup at home.
During a medical assessment, the doctor:
- Observe the child's breathing patterns
- Listens to the chest using a stethoscope
- Examines the child's throat
- Sometimes, doctors may order additional tests to rule out other illnesses. These may include:
- X-rays of the neck and chest
- Laboratory tests
It's important to note that such tests are rarely necessary. Most cases of croup can be diagnosed through observation and physical examination alone.
Treatment for Croup
The croup treatment depends on the severity of the child's condition.
For mild croup, parents can try the following:
- Keep the child calm and comfortable
- Use a cool-mist humidifier or sit with the child in a steamy bathroom
- Ensure proper hydration
Doctors may suggest the following medical management for moderate to severe cases:
- Corticosteroids: To reduce airway swelling
- Nebulised epinephrine: An inhaled treatment to quickly reduce airway inflammation
- Oxygen therapy: To improve breathing in severe cases
- Doctors may administer a single dose of oral dexamethasone, which typically starts working within six hours. For children who can't keep medicine down, intravenous or intramuscular injections are options.
In rare, severe cases, a child may need to be hospitalised for closer monitoring and possible mechanical ventilation. However, with prompt and appropriate croup disease treatment, most children with croup recover quickly.
Risk Factors for Croup
Several factors increase a child's likelihood of developing this condition, such as:
- Age: Children between 6 months and three years of age face the highest risk. Their small airways make them more prone to severe symptoms.
- Gender: Boys and children assigned male at birth (AMAB) are more likely to develop croup compared to girls and children assigned female at birth (AFAB).
- Anatomical factors: A narrowing in the airway, either present from birth or developed later, can increase susceptibility to the infection. If a child experiences repeated episodes of croup, it may signal an underlying airway issue.
Complications of Croup
While croup is usually mild and self-limiting, complications can occur in rare cases. Less than 5% of children with croup require hospitalisation.
The most common reasons for hospitalization include:
- Need for oxygen therapy to maintain safe oxygen levels
- Severe dehydration requiring intravenous fluid therapy
- Persistent severe croup disease symptoms despite initial treatment
- Sometimes, a child's breathing may become fatigued, necessitating closer monitoring and more intensive care.
Uncommon but serious complications can include:
- Bacterial tracheitis: A bacterial infection of the windpipe
- Pneumonia: Infection of the lungs
- Pulmonary oedema: Fluid accumulation in the lungs
When to See a Doctor
Parents should seek emergency medical care if:
- If a child's symptoms worsen or persist
- The child's fever lasts for more than three days
- The child is younger than 12 weeks and has a fever of 38°C (100.4°F) or higher
- The child coughs nonstop or has persistent noisy breathing when still
- The cough lasts for more than ten days
- The child has difficulty breathing, speaking, or drinking
- If a child shows blue-tinged skin around the mouth or fingernails
- The child drools excessively or can't swallow
- If a child experiences severe coughing spells
- The child has a high-pitched whistling sound while breathing (stridor)
- If a child shows chest retractions (skin pulling in around ribs and breastbone)
- The child struggles to breathe, speak, or drink
- Their lips or face turn bluish
Home Remedies for Croup
Parents can manage mild cases of croup at home with several effective remedies, including:
- Keeping the child calm is crucial, as crying and agitation can worsen symptoms. Offering comfort through cuddles, favourite toys, or soothing activities helps reduce distress.
- Sitting in a steamy bathroom or a cool-mist humidifier can help relax the vocal cords and reduce inflammation.
- Some parents find that exposing the child to cool air, either outdoors or in front of an open freezer, provides relief.
- Proper hydration is essential. Warm fluids like milk or cool options like water and popsicles can soothe the throat and prevent dehydration. For children over 12 months, a spoonful of honey may help ease coughing.
- Positioning the child in an upright or slightly forward-leaning posture can improve breathing. Creating a 'pillow fort' for sleep or holding the child upright may provide comfort.
- Parents can use over-the-counter medications for fever or discomfort, following age-appropriate dosage guidelines. However, cough medicines are not recommended for young children.
Prevention
Parents can take several steps to prevent croup and reduce its spread, such as:
- Frequent hand-washing with soap and water for at least 20 seconds stands as the most crucial measure.
- Keeping children away from sick individuals and encouraging them to cough or sneeze into their elbows also helps limit transmission.
- To maintain a healthy environment:
- Clean frequently touched surfaces regularly
- Wash toys between each use
- Throw used tissues away promptly
- During outbreaks, keeping children home from school or daycare is advisable. This practice helps contain the spread of the virus.
- Vaccination plays a vital role in prevention. While there isn't a vaccine specifically for parainfluenza viruses, keeping children's vaccinations up to date offers protection against some rare but dangerous upper airway infections. The Haemophilus influenzae type b (Hib) vaccines and diphtheria are essential in this regard.
Conclusion
Croup can be a concerning condition for parents, but understanding its symptoms and treatment options helps manage it effectively. The distinctive barking cough, often accompanied by difficulty breathing, is a clear indicator of croup in young children. While parents can handle most cases at home with simple remedies like cool mist and proper hydration, it's crucial to recognise when medical attention becomes necessary. With prompt recognition and appropriate care, most children recover quickly from croup, allowing families to navigate this common childhood illness confidently.
FAQ's
1. Is Steam good for croup?
While many parents believe steam helps with croup, there's no scientific evidence to support this. Some find that sitting with their child in a steamy bathroom improves breathing, but studies haven't proven its effectiveness. Cool mist humidifiers are often recommended instead of hot vaporisers to avoid the risk of burns.
2. Is a nebulizer good for croup?
For moderate to severe croup, nebulised treatments can be beneficial. Epinephrine, administered through a nebuliser, reduces airway swelling quickly, usually within 10 minutes.
3. What to do with croup at night?
Croup symptoms often worsen at night. Parents can use a cool mist humidifier in the child's room or take them outside to breathe cool, moist night air. It's advisable to stay close to the child to provide immediate assistance if breathing difficulties occur. Keeping the child calm is crucial, as anxiety can exacerbate symptoms.
4. When to worry about croup?
Parents should seek immediate medical intervention if their child:
- Has difficulty breathing or speaking
- Shows blue-tinged lips or fingernails
- Has stridor (noisy breathing) even when resting
- Drools excessively or struggles to swallow
- Experiences severe coughing spells
5. What is the best medicine for croup?
Corticosteroids are highly effective in treating croup. They reduce airway swelling, typically within six hours of the first dose. For mild cases, a single dose may suffice. Doctors might prescribe additional doses or combine it with other treatments like nebulised epinephrine in more severe cases.
6. What age does croup stop?
Croup most commonly affects children between 6 months and three years old. As children grow, their airways widen, making them less susceptible to the breathing difficulties caused by croup. The condition rarely occurs in children over six years of age.
Still Have a Question?




