-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Costochondritis
Symptom, Causes, Diagnosis and Treatment
Costochondritis
Have you ever experienced a sharp and stabbing pain in the chest or thoracic region that worsens when you breathe deeply or move? It could be a sign of costochondritis. It is a condition that affects the cartilage connecting your ribs to your breastbone.
Costochondritis can cause significant discomfort and worry, as its symptoms often mimic those of more serious heart conditions. Understanding this condition is crucial for those who suffer from it, as proper diagnosis and treatment can significantly improve quality of life.
Understanding this condition is crucial for those who suffer from it, as proper diagnosis and treatment can significantly improve quality of life. This article will explore the various costochondritis pain locations, discuss effective costochondritis treatment options, and provide insights into when you should see a doctor.
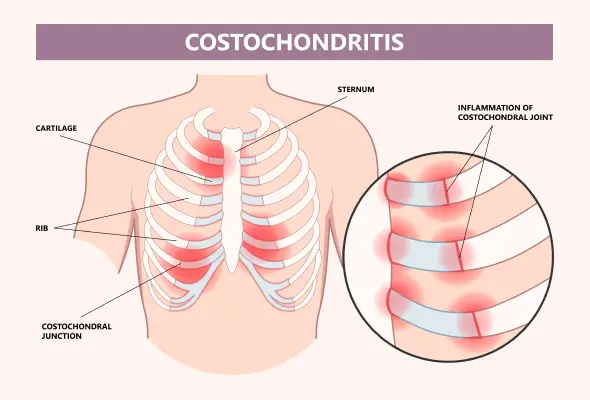
What is Costochondritis?
Costochondritis is a common condition that causes inflammation in the cartilage that connects the breastbone (sternum) to the ribs. This inflammation leads to chest pain, which can be severe and often mistaken for a heart attack. However, costochondritis is typically harmless and self-limiting. It affects the costochondral joints, which protect vital organs like the heart and lungs. The pain associated with costochondritis can start suddenly or develop gradually, potentially spreading across the chest. It usually worsens with movement, deep breathing, or coughing. Costochondritis most commonly affects adults aged 40 to 50 years and is estimated to occur in 4% to 50% of patients with chest pain.
Causes of Costochondritis
The exact cause of costochondritis often remains unclear. However, several factors may contribute to its development, such as:
- Infections in the chest area can lead to inflammation of the costochondral joints.
- Repeated minor trauma to the chest wall, such as from intense physical activity or sudden increases in workout intensity, can also trigger this condition.
- Severe coughing or vomiting episodes may strain the chest, potentially causing costochondritis.
- In some cases, inflammatory diseases affecting joints and the spine, like arthritis, can impact the cartilage in the chest area.
- Costochondritis might also be associated with seronegative spondyloarthropathies or thoracic tumours.
- Intravenous drug abuse has been linked to this condition as well.
Symptoms of Costochondritis
- Costochondritis primarily causes chest pain, which is the most common symptom. This pain is typically concentrated on the left side of the breastbone and can be sharp, aching, or feel like pressure.
- Pain may affect multiple ribs and radiate to the arms and shoulders.
- The discomfort often worsens when taking deep breaths, coughing, sneezing, or vomiting.
- Certain activities can also exacerbate the costochondritis pain. These may include hugging, exercising, and lying on the affected side.
- The duration of costochondritis symptoms varies, typically lasting from a few days to several weeks. In rare cases, the discomfort may persist for months.
- It's crucial to note that costochondritis pain can mimic that of a heart attack, making it essential to seek medical attention if you experience persistent or worsening chest pain.
Risk Factors
While costochondritis can affect anyone, certain groups have a higher risk of contracting this condition, such as:
- Athletes who participate in contact sports
- Individuals with physically demanding jobs
- Females and individuals assigned female at birth (AFAB) also have a higher risk, particularly those who are athletes.
- Age plays a role, with adults over 40-50 being more susceptible.
- People of Hispanic ancestry have shown a higher incidence of costochondritis.
- Recent physical trauma to the chest area
- Frequent exposure to irritants for those with allergies
- Individuals with rheumatologic disorders
- People who engage in intravenous drug abuse
Diagnosis
Diagnosing costochondritis involves a process of elimination. Doctors perform a thorough physical assessment, focusing on the chest wall. They may press on the chest to pinpoint areas of tenderness, which is often reproducible in costochondritis. The examination also includes assessing the effect of deep breathing and upper body movements on pain.
While there's no specific test for costochondritis, doctors may conduct:
- Blood tests to rule out infections
- Imaging tests like chest X-rays, CT scans, or MRIS to exclude other conditions
- An electrocardiogram (ECG) to rule out cardiac issues
Treatment for Costochondritis
Treatment for costochondritis focuses on pain relief, as the condition usually resolves on its own.
- Rest is crucial, allowing the irritated costochondral joints to heal.
- Applying heat or ice compress to the affected area may also provide relief.
- Over-the-counter pain relievers can help manage discomfort.
- In some cases, doctors might prescribe stronger medications such as prescription- strength NSAIDs or, rarely, corticosteroid injections for persistent symptoms.
- Gentle stretching exercises for the chest muscles can be beneficial. These may include doorway stretches or using a foam roller.
- It's important to avoid activities that worsen pain and to visit a doctor if symptoms persist or worsen.
When to See a Doctor
While costochondritis often resolves on its own, seeking medical attention in certain situations is crucial, such as:
- If you experience persistent or severe pain in the chest
- If you have trouble breathing, a high fever, or signs of infection such as pus, redness, or swelling around your ribs, contact your doctor immediately.
- If your pain worsens or doesn't improve with medication
- If you have sharp pain with every breath
Preventions
While it may not be possible to prevent costochondritis entirely, you can take steps to reduce your risk, such as:
- Proper posture is crucial, especially during activities that strain the chest muscles.
- Avoid repetitive movements that put pressure on the chest area.
- Before exercising, warm up and stretch to prepare your muscles.
- When lifting heavy objects, use the correct techniques to avoid excessive strain.
- Wearing protective gear during activities with a risk of chest trauma can also help.
- Promptly treating respiratory infections may lower the chances of developing costochondritis as a complication.
- If you've had costochondritis before, regularly performing stretching and postural exercises can help keep symptoms under control.
Remember to rest after intense physical activity to give your body time to recover and minimise stress on your chest and ribs.
Conclusion
Costochondritis, while often a cause for concern, is generally a manageable condition with the right approach. Understanding its symptoms, reasons, and treatment options is critical to effectively dealing with this chest wall inflammation. Rest, over-the-counter pain relievers, and gentle stretching exercises often provide relief for most people. However, it's crucial to remember that you should not take chest pain lightly, and seeking medical guidance is essential to rule out more serious conditions.
Taking steps to prevent costochondritis can go a long way in maintaining chest health. By staying informed and proactive, individuals can better manage this condition and enhance their overall quality of life.
FAQ's
1. Is costochondritis dangerous?
Costochondritis is generally not dangerous. It's a benign condition causing chest wall pain due to inflammation of the cartilage connecting ribs to the breastbone. While the pain can be severe and mimic heart attack symptoms, it's typically harmless and self- limiting. However, seeking medical attention for chest pain is crucial to rule out more serious conditions.
2. What can I expect if I have costochondritis?
If you have costochondritis, you can expect chest pain that may be sharp, aching, or feel like pressure. The discomfort often worsens with deep breathing, coughing, or movement. Most people experience symptoms for a few days to several weeks, with full recovery expected.
3. How long does costochondritis last?
Costochondritis typically lasts for several weeks to a few months. In most cases, it resolves within 6-8 weeks. However, some individuals may experience chronic or recurring symptoms that can persist for longer periods.
4. What is the difference between costochondritis vs. Tietze syndrome?
While both conditions involve inflammation of the costal cartilage, there are key differences:
- Costochondritis:
- Affects multiple rib joints
- No noticeable swelling
- More common and typically affects adults
- Tietze syndrome:
- Usually affects one rib joint, often the second or third
- Characterised by visible swelling at the affected area
- Less common and typically affects younger individuals
5. Can costochondritis be cured?
Costochondritis often resolves on its own over time. While there's no specific "cure," treatment focuses on managing symptoms and promoting healing:
- Rest and avoid activities that exacerbate pain
- Over-the-counter pain relievers and anti-inflammatory medications
- Heat or cold therapy
- Gentle stretching exercises
- In some cases, corticosteroid injections for severe pain
Most people experience significant improvement with conservative treatment.
6. What foods trigger costochondritis?
Specific foods do not typically trigger costochondritis. However, some individuals report that certain dietary choices may influence inflammation in the body, potentially affecting their symptoms:
- Foods high in trans fats & saturated fats
- Processed foods and refined sugars
- Alcohol
While there's no direct link between diet and costochondritis, maintaining a balanced, anti-inflammatory diet enriched in vegetables, fruits, and omega-3 fatty acids may support overall health and reduce inflammation.
7. Does stress cause costochondritis?
Stress itself doesn't directly cause costochondritis, but it can play a role in exacerbating symptoms:
- Stress can increase muscle tension, potentially aggravating existing inflammation
- Stress may lower pain tolerance, making symptoms feel more intense
- Anxiety related to chest pain can lead to shallow breathing, which may worsen the discomfort
While stress reduction techniques may help alleviate symptoms, it's important to note that costochondritis has various potential causes beyond stress.
8. Who is at risk for costochondritis?
Several factors can increase the likelihood of developing costochondritis:
- Age and gender: More common in young adults and adolescents, particularly females
- Physical activity: Athletes or those engaged in repetitive upper body movements
- Respiratory conditions: People with chronic cough or upper respiratory infections
- Trauma: Previous chest trauma or surgery
- Certain medical conditions: Fibromyalgia, rheumatoid arthritis, or other inflammatory disorders
- Poor posture: Can contribute to chest wall stress
Still Have a Question?




