-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Corneal Ulcer
Symptom, Causes, Diagnosis and Treatment
Corneal Ulcer
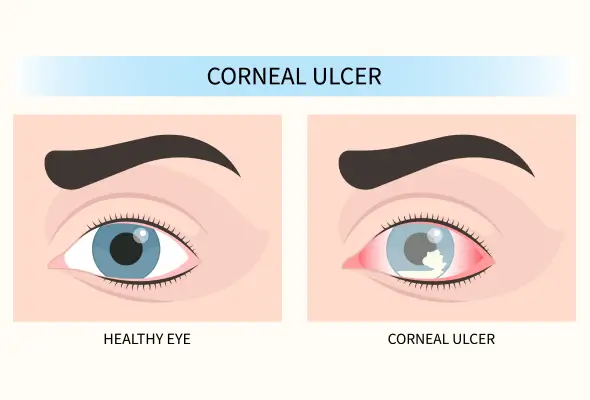
A corneal ulcer can threaten vision if left untreated. This serious eye condition affects the cornea—the clear front surface of the eye—and requires immediate medical attention to prevent permanent vision loss. Early recognition of corneal ulcer symptoms and prompt treatment significantly improve the possibility of complete recovery. Modern corneal ulcer treatment options have made it possible to save vision in most cases when patients seek help quickly.
What Is a Corneal Ulcer (Keratitis)?
A corneal ulcer, known as keratitis, is an open sore that develops on the cornea—the clear, dome-shaped tissue layer at the front of the eye. This condition occurs when there is a loss of corneal tissue, often accompanied by inflammation. Doctors consider corneal ulcers an ophthalmologic emergency due to their potential to cause permanent vision damage if left untreated.
Symptoms of Corneal Ulcer
The following are most common symptoms of corneal ulcers:
- Redness or bloodshot appearance in the affected eye
- Excessive tearing or watery eye (epiphora)
- Eye pain ranging from mild discomfort to severe aching
- Foreign body sensation, similar to having dust or an eyelash in the eye
- Light sensitivity (photophobia)
- Blurred or decreased vision
- Swollen eyelids
Risk Factors and Causes of Corneal Ulcers
The development of corneal ulcers stems from various causes, with infections being the primary trigger. These infections typically occur when the protective outer layer of the cornea becomes compromised, allowing harmful organisms to penetrate the eye tissue.
Infectious causes include:
- Bacterial Infections: Contact lens wear significantly increases the risk of developing corneal ulcers, especially with extended-wear soft lenses. The risk becomes ten times higher when these lenses are worn overnight.
- Viral Infections: Caused by herpes simplex virus or varicella virus
- Fungal Infections: Often resulting from plant material entering the eye
- Parasitic Infections: Particularly from Acanthamoeba, found in fresh water and soil
Non-infectious causes are:
- Chemical burns
- Autoimmune conditions
- Toxic reactions
- Neurotrophic causes
Several other factors can elevate the likelihood of developing corneal ulcers, including:
- Dry eyes
- Eyelid disorders that prevent proper closure
- Bell's palsy
- Corneal injuries
- Severe allergic eye conditions
- Type 2 diabetes or those using steroid eye drops
- A history of eye surgery or corneal diseases
Complications of Corneal Ulcer
Several complications can develop if a corneal ulcer remains untreated or receives inadequate treatment:
- Corneal Scarring: Permanent marks on the cornea that can affect vision clarity
- Vision Changes: Development of irregular astigmatism affecting eyesight
- Structural Problems: Risk of corneal perforation (holes in the cornea)
- Secondary Conditions: Development of serious eye conditions including:
- Glaucoma (increased eye pressure)
- Cataracts (clouding of the eye lens)
- Endophthalmitis (severe internal eye infection)
Diagnosis
The diagnostic process includes a thorough examination using a specialised instrument called a slit-lamp biomicroscope, which allows detailed visualisation of the cornea's surface.
The eye specialist typically performs several key diagnostic tests:
- Fluorescein Staining: Special dye highlights damaged areas of the cornea
- Corneal Culture: Samples from the ulcer help identify specific infections
- Confocal Microscopy: Provides detailed images of corneal cells
- High-definition Photography: Documents the ulcer's appearance and progression
- Laboratory Investigations: They may be necessary when underlying conditions like rheumatoid arthritis, lupus, or other autoimmune disorders are suspected.
- Corneal Topography and Anterior Segment OCT: These tests provide detailed information about the ulcer's depth and extent.
Treatment
Treatment options for corneal ulcers depend on the underlying cause identified during diagnosis. The main treatment approaches include:
- Medications:
- Antibiotic eye drops for bacterial infections
- Antiviral medicines for viral infections
- Antifungal treatments for fungal ulcers
- Special medications for parasitic infections
- Anti-inflammatory Treatment:
- Corticosteroid eye drops to reduce inflammation
- Used carefully under medical supervision
- Often combined with antimicrobial therapy
- Surgery: For severe cases that don't respond to medication, surgical intervention may be necessary. A corneal transplant involves removing and replacing the damaged cornea with healthy donor tissue. Doctors typically recommend this procedure for cases where medication alone proves insufficient.
When to See a Doctor
Immediate medical attention is necessary if patients experience:
- Severe eye pain, especially following trauma
- Sudden vision changes or blurred vision
- Intense light sensitivity affecting daily activities
- Significant eye discharge
- Symptoms that worsen despite ongoing treatment
- Pressure in the eye accompanied by nausea
- Vision problems with fever or chills
- Inability to move eyes normally
- Bulging of the eyeball
Prevention
Preventing corneal ulcers involves implementing proper eye care practices and maintaining good hygiene.
Essential preventive measures include:
- Maintaining proper hand hygiene before touching eyes
- Using protective eyewear during high-risk activities
- Following a balanced diet rich in vitamins
- Staying adequately hydrated throughout the day
- Taking regular breaks during screen time using the 20-20-20 rule
- Avoiding exposure to water while wearing contact lenses
- Replacing contact lens cases every 1-3 months
- Wearing sunglasses with UV400 or 100% UV protection when outdoors
Conclusion
Corneal ulcers remain a serious eye condition that demands quick medical attention and proper treatment. Medical advances have made successful treatment possible, especially when patients seek care early. Combining appropriate medication, careful monitoring, and proper eye care leads to positive patient outcomes.
FAQs
1. What are the earliest symptoms of corneal ulcers?
The earliest signs of a corneal ulcer typically include redness and a watery eye. Patients often experience a foreign body sensation, as if something is stuck in their eyes. Light sensitivity and mild discomfort may also occur before more severe symptoms develop.
2. Is a corneal ulcer curable?
Most corneal ulcers are curable with proper medical treatment. The healing process typically takes two to three weeks with appropriate medication. However, success depends on early intervention and carefully following the prescribed treatment plan.
3. What is the fastest way to heal an eye ulcer?
The most effective healing approach involves immediate medical attention and strict adherence to prescribed treatments. Patients should:
- Remove contact lenses immediately
- Use prescribed antibiotics or antifungal medications as directed
- Avoid rubbing or touching the affected eye
- Attend all follow-up appointments
4. What are the four stages of a corneal ulcer?
Corneal ulcers progress through four distinct stages:
- Epithelial defect: Initial damage to the cornea's outer layer
- Stromal infiltration: Infection spreading to deeper layers
- Descemetocele: Ulcer reaching the cornea's innermost layer
- Corneal perforation: Complete penetration through the cornea
5. What foods are good for corneal ulcers?
A nutrient-rich diet supports corneal healing. Beneficial foods include:
- Eggs (rich in vitamin A and zinc)
- Fish (containing omega-3 fatty acids)
- Citrus fruits (high in vitamin C)
- Leafy greens like kale (containing lutein and zeaxanthin)
- Almonds (source of vitamin E)

Still Have a Question?



