-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Colitis
Symptom, Causes, Diagnosis and Treatment
Colitis
Have you ever experienced persistent abdominal pain or frequent trips to the bathroom? These could be signs of colitis, a condition that affects millions worldwide. Colitis involves inflammation of the colon lining, causing discomfort and disrupting daily life.
What is Colitis?
Colitis is a condition characterised by inflammation of the colon, which is the main part of the large intestine. This inflammation affects the lining of the colon, causing discomfort and disrupting the final stages of digestion. The colon plays an elementary role in the digestive process, serving as the last leg of the travel the food takes through the digestive system.
Types of Colitis
Colitis comes in various forms, each with distinct causes and characteristics, such as:
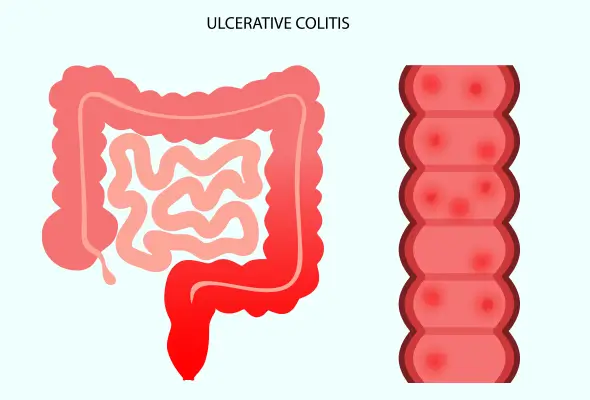
- Ulcerative colitis (UC)
- Pseudomembranous colitis
- Ischemic colitis
- Microscopic colitis
- Allergic colitis
- Infectious colitis
- Radiation colitis
- Diversion colitis
Symptoms of Colitis
In the early stages, individuals may experience diarrhoea, which may or may not contain blood. Increased bowel movements, typically four or fewer episodes daily, become common. Urgent bowel movements and tenesmus, a feeling of needing to defecate without being able to, also occur. Mild abdominal cramping or tenderness may accompany other colitis disease symptoms.
As the condition progresses, moderate to severe colitis symptoms can develop. These include more frequent bowel movements, often exceeding four episodes daily. Blood, mucus, or pus may appear in the stool. Severe abdominal cramping becomes more pronounced, and individuals may experience fatigue, sudden weight loss, nausea, and fever.
Causes of Colitis
Different types of colitis have various causes, such as:
- Infectious colitis stems from viral, parasitic, or bacterial infections, often contracted through contaminated food or water. Salmonella and E. coli are common culprits.
- Pseudomembranous colitis usually results from C. diff overgrowth, ironically triggered by antibiotic use.
- Allergic colitis affects breastfed babies due to food intolerances, typically to dairy or soy proteins in breast milk.
- Ischemic colitis occurs when intestinal blood supply becomes insufficient, usually caused by blood vessel blockages like clots or atherosclerosis.
- Inflammatory bowel diseases, including ulcerative colitis and microscopic colitis, have no direct cause. Doctors believe they are autoimmune conditions, partially genetic and triggered by environmental factors.
- Radiation colitis is a side effect of cancer treatment.
- Diversion colitis can occur after a colostomy.
Diagnosis
Initially, doctors review the patient's medical history and perform a physical examination. During this exam, they check for signs like paleness, which may indicate anaemia and abdominal tenderness caused by inflammation. They also listen to sounds within the abdomen using a stethoscope.
- Blood tests help identify signs of colitis and related complications. These tests can reveal anaemia, inflammation, or signs of infection.
- Analysis of stool samples helps rule out infections that might cause similar symptoms.
- If inflammatory bowel disease is suspected, further tests are necessary. These include:
- Endoscopic Procedures: Colonoscopy and flexible sigmoidoscopy allow doctors to view the colon's lining and take tissue samples for biopsy.
- Imaging Tests: X-rays, CT scans, or MR enterography help rule out complications and assess the extent of inflammation.
- Tissue Biopsy: This is crucial for a definitive diagnosis of ulcerative colitis.
Treatment
The approach to treating colitis depends on its type and severity. Doctors often start with medications to manage colitis symptoms and reduce inflammation.
- Anti-inflammatory drugs are typically the first line of colitis treatment.
- For more severe cases, doctors may recommend corticosteroids to suppress the immune system & reduce inflammation quickly.
- Immunosuppressants are used when other treatments fail.
- Biologics, a newer class of drugs, target specific proteins in the immune system.
Risk Factors for Colitis
Colitis involves a complex interplay of factors that increase one's susceptibility to the condition.
- Age plays a significant role, with most diagnoses occurring between 15 and 30 years old or after 60.
- Race and ethnicity also influence risk, with white individuals facing a higher likelihood of developing colitis.
- A person with a blood relative (parent, sibling, or child) who has ulcerative colitis or
- Crohn's disease is more prone to developing the condition.
Complications of Colitis
Colitis can lead to various complications that affect both the digestive system and other parts of the body, including:
- About one in three people with ulcerative colitis experience inflammation beyond the intestines, known as extra-intestinal manifestations. These can impact bones, joints, skin, and eyes.
- Colitis patients become more susceptible to developing osteoporosis. This condition causes weak bones, making them more prone to fractures.
- Colitis and its treatments can affect growth and delay puberty in children.
- Colitis also increases colon cancer risk, especially in cases of severe or long-standing inflammation.
- In emergencies, colitis can cause life-threatening complications such as colon perforation, severe bleeding requiring transfusion, and toxic megacolon.
When to See a Doctor
Individuals experiencing persistent diarrhoea, blood in their stools, or constant pain with a high fever should contact their doctor immediately. These symptoms don't necessarily indicate colitis, but they warrant medical attention.
Prevention
While it's not possible to completely prevent colitis flare-ups, individuals can take steps to manage their condition and reduce the likelihood of symptoms worsening.
- One of the most effective strategies is to identify and avoid triggers. This often involves keeping a daily food journal to track dietary choices and their effects on symptoms. For many people with colitis, certain foods can exacerbate symptoms. Common triggers include lactose products, red and processed meats, alcohol, carbonated drinks, sugary foods, high-fat foods, and spicy foods. However, it's important to note that triggers can vary from person to person. Working with a gastroenterologist and dietician to develop a personalised meal plan can help individuals avoid trigger foods without compromising essential nutrients.
- Stress management plays a huge role in preventing flare-ups. Regular exercise, getting at least seven hours of sleep each night, and practising relaxation techniques like meditation or yoga can help reduce stress levels.
- Medication management is another key aspect of prevention. Taking prescribed medications exactly as directed is vital for keeping colitis in check. It's also important to be cautious with certain over-the-counter medications, particularly NSAIDs, which can worsen symptoms.
Conclusion
Colitis management involves a combination of medical treatments, lifestyle adjustments, and ongoing care. People can improve their quality of life by working closely with their gastroenterologist, identifying triggers & staying informed about the latest developments in colitis research. Remember, while colitis can be challenging, with proper care and support, many people lead fulfilling lives despite this condition.
FAQ's
1. Is colitis a serious disease?
Colitis is a chronic inflammatory bowel condition that can be serious. While it's not usually life-threatening, it can increase the risk of severe complications, especially if it doesn't respond to treatment.
2. Does colitis go away?
Colitis doesn't go away completely, but it can be managed. The condition often involves periods of symptom flare-ups followed by periods of remission. With appropriate treatment, many people achieve long-term remission.
3. What is the main cause of colitis?
The exact cause of colitis remains unclear. However, researchers believe it involves a complex interplay of factors, including:
- Genetics: Certain genes may increase susceptibility.
- Immune System Dysfunction: An abnormal immune response may lead to inflammation in the colon.
- Environmental Factors: Westernised dietary patterns, lifestyles, and triggers like smoking or air pollution may contribute.
4. Should I worry about colitis?
While colitis is a serious condition, it's manageable with proper care. However, it's essential to be aware of potential complications.
5. What food to avoid with colitis?
People with colitis should generally avoid:
- High-fibre foods (raw green vegetables, whole nuts, whole grains)
- Lactose products (for those with lactose intolerance)
- Red and processed meats
- Alcohol and carbonated drinks
- Sugary foods and sugar alcohols
- High-fat foods
- Spicy foods
- Gluten (for some individuals)
6. How painful is colitis?
Colitis pain can vary significantly among individuals-about 33% of people with colitis experience chronic abdominal pain. The pain often occurs in the rectum and lower left side of the abdomen. During flare-ups, people may experience cramping, urgency, and discomfort during bowel movements.

Still Have a Question?



