-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Cirrhosis
Symptom, Causes, Diagnosis and Treatment
Cirrhosis
Cirrhosis is a serious liver condition that affects millions of people worldwide. It is a progressive liver disease. This means it can lead to severe complications if left untreated. Understanding the liver cirrhosis reasons, manifestations, and treatment options for cirrhosis is crucial for maintaining good liver health and preventing further damage. Let's explore the various aspects of cirrhosis and its management so you know how to control your liver health.
What is Cirrhosis of the Liver?
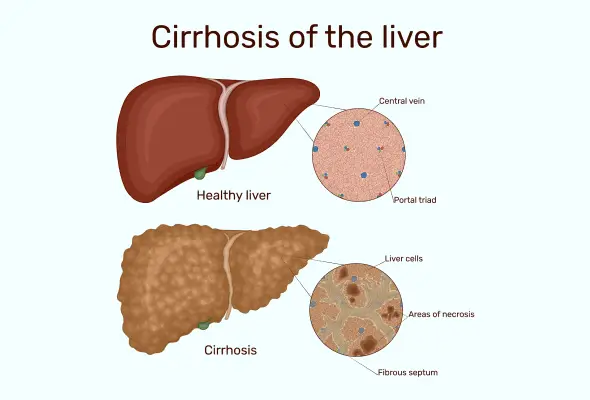
Cirrhosis is a chronic liver disease in which unhealthy scar tissue replaces healthy liver tissue. This scarring process impairs the liver's ability to function correctly, leading to various health issues. The liver is an organ necessary for human survival and responsible for numerous functions, including the metabolism of drugs, the production of blood- clotting proteins, and the removal of toxins from the body. When cirrhosis develops, the liver's capacity to perform these critical tasks is compromised, putting the individual's overall health at risk.
Symptoms of Liver Cirrhosis
The cirrhosis symptoms can vary widely and depend on the stage and severity of the condition. In the early stages, individuals may not experience any noticeable symptoms, as the liver is able to compensate for the damage. However, as the disease progresses, the following symptoms may become more prevalent:
- Fatigue and weakness
- Loss of appetite and unintentional weight loss
- Abdominal pain or discomfort
- Swelling in the legs or abdomen (oedema)
- Jaundice (yellowing of the skin and eyes)
- Itchy skin
- Bruising and bleeding easily
- Mental confusion or changes in behaviour (hepatic encephalopathy)
- Nausea and vomiting
- Diarrhoea
- Dark-coloured urine and light-coloured poop
- Small yellow nodules of fat deposits on your skin or eyelids
Causes of Liver Cirrhosis
Various factors can cause cirrhosis, and getting to the root cause of this condition is the first step to effective liver cirrhosis treatment & prevention. The most common causes of liver cirrhosis are:
- Chronic Alcohol Abuse: Long-term, excessive alcohol consumption is one of the leading liver cirrhosis causes, as alcohol can directly damage and inflame the liver.
- Viral Hepatitis: Chronic viral hepatitis (particularly hepatitis B & C) can lead to cirrhosis over time.
- Nonalcoholic Fatty Liver Disease (NAFLD): This condition is characterised by fat buildup in the liver. It can progress to a more severe form with time called nonalcoholic steatohepatitis (NASH), which can ultimately result in cirrhosis.
- Autoimmune Disorders: Certain autoimmune diseases, such as primary biliary cholangitis & primary sclerosing cholangitis, can cause inflammation as well as scarring in the liver, leading to cirrhosis.
- Genetic Disorders: Rare genetic disorders, such as Wilson's disease and hemochromatosis, can also contribute to the development of cirrhosis.
- Bile Duct Blockage: Blockages or damage to the bile ducts (a tube-like structure responsible for bile transportation from the liver to the small intestine) can lead to cirrhosis.
- Chronic Heart Failure: In some cases, cirrhosis can develop as a result of chronic heart failure, which can impair the liver's ability to function correctly.
Stages of Cirrhosis of the Liver
Cirrhosis is a progressive disease, and it can have categories depending on the degree of liver damage and the associated complications of cirrhosis. The stages or types of liver cirrhosis are as follows:
- Early-Stage Cirrhosis: At this stage, the liver is still able to function relatively well, and there may be few or no noticeable symptoms. However, the scarring process has already begun, and the liver's ability to perform its essential tasks gradually diminishes.
- Compensated Cirrhosis: In this stage, the liver is still able to compensate for the damage, and the individual may not experience any apparent symptoms. However, the liver's capacity to perform its functions is significantly reduced, and the risk of complications increases.
- Decompensated Cirrhosis: As the disease progresses, the liver can no longer compensate for the damage, and various complications begin to arise. These may include fluid buildup in the abdomen (ascites), bleeding from enlarged veins in the oesophagus or stomach (varices), and changes in mental function (hepatic encephalopathy).
- End-Stage Cirrhosis: At this advanced stage, the liver is severely damaged, and the individual's life is at risk. Complications become increasingly severe, and the only viable cure for cirrhosis liver may be a liver transplant.
Diagnosis of Cirrhosis
Diagnosing cirrhosis involves a combination of various tests and examinations. The process may include:
- Medical History and Physical Examination: The treating physician will ask about the individual's medical history, including any underlying conditions, and perform a detailed physical examination to observe signs of liver disease, such as jaundice or abdominal swelling.
- Blood Tests: Blood investigations can help detect abnormalities in liver function (elevated levels of certain enzymes or proteins), which may indicate the presence of cirrhosis.
- Imaging Tests: Techniques like ultrasound, CT scan, or MRI provide a comprehensive set of images of the liver, allowing your physician to assess the extent of damage and scarring.
- Liver Biopsy: Sometimes, a small sample of liver tissue may be taken and analysed under a microscope. A biopsy can be a confirmatory test for the diagnosis and determining the underlying cause of cirrhosis.
- Endoscopy: If the doctor suspects the presence of enlarged veins in the oesophagus or stomach (varices), they may perform an endoscopic examination to assess the risk of bleeding.
Treatment for Liver Cirrhosis
The treatment for liver cirrhosis depends on the underlying cause, the stage of the disease, and the presence of any associated complications. Some common treatment approaches include:
- Addressing the Root Cause: If the cause of cirrhosis is identified, such as chronic alcohol abuse or viral hepatitis, the doctor will focus on treating the underlying condition to halt the progression of the disease.
- Lifestyle Changes: Adopting healthy lifestyle choices, including but not limited to a balanced diet, exercise, and a complete no to alcohol, can slow the progression of cirrhosis & prevent further liver damage.
- Medication: Certain medicines can manage the symptoms of cirrhosis, such as diuretics to reduce fluid buildup, laxatives to address constipation, and antibiotics to treat infections.
- Liver Transplantation: In cases of advanced, end-stage cirrhosis, a liver transplant procedure may be the only viable treatment option.
- Supportive Care: Depending on the individual's needs, supportive care measures may include nutritional support, management of complications, and pain relief.
Risk Factors for Liver Cirrhosis
Certain factors can increase an individual's risk of developing cirrhosis, including:
- Long-term, heavy alcohol use is one of the leading causes of cirrhosis.
- Long-standing infection with hepatitis B or C viruses can significantly increase the risk of developing cirrhosis.
- Metabolic conditions like nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH) can lead to cirrhosis.
- Certain autoimmune diseases (primary biliary cholangitis & primary sclerosing cholangitis) can cause liver inflammation and scarring, leading to cirrhosis.
- Rare genetic disorders, like Wilson's disease and hemochromatosis, can predispose individuals to the development of cirrhosis.
- Prolonged exposure to certain toxins, such as industrial chemicals or certain medications, can contribute to the development of cirrhosis.
- Individuals with chronic heart failure may be at an increased risk of developing cirrhosis due to its impact on liver function.
Complications of Liver Cirrhosis
Cirrhosis can lead to a range of serious complications that can impact an individual's health and quality of life, such as:
- Ascites: The fluid buildup in the abdominal cavity can cause swelling and discomfort.
- Variceal Bleeding: The enlarged veins in the oesophagus or stomach can rupture and cause severe bleeding.
- Hepatic Encephalopathy: Changes in mental function, ranging from confusion to coma, due to the buildup of toxins in the body.
- Liver Cancer: Individuals with cirrhosis have an increased risk of developing hepatocellular carcinoma.
- Kidney Failure: Cirrhosis can lead to the development of kidney problems, including acute or chronic kidney failure.
- Infections: Individuals with cirrhosis are more susceptible to infections.
- Bleeding and Clotting Disorders: Cirrhosis can impair the liver's ability to produce blood-clotting proteins, leading to an increased risk of bleeding and bruising.
When to See a Doctor
If you or someone you know is experiencing symptoms that may be related to liver cirrhosis, talk to your doctor immediately. These symptoms can be:
- Persistent fatigue or weakness
- Unexplained weight loss or loss of appetite
- Abdominal pain or discomfort
- Swelling in the legs or abdomen
- Yellowing of the skin or eyes (jaundice)
- Easy bruising or bleeding
- Changes in mental function (confusion or disorientation)
Prevention of Liver Cirrhosis
While some risk factors for cirrhosis cannot be controlled (genetic disorders), there are several steps one can take to reduce the risk & prevent the development of this condition:
- Avoiding excessive alcohol consumption or abstaining from alcohol
- Maintaining a healthy lifestyle, including adopting a balanced diet, engaging in regular physical activity
- Manage underlying health conditions
- Reducing exposure to harmful chemicals, industrial pollutants, and certain medications that can damage the liver
- Get vaccinated, as vaccination against hepatitis B can help prevent the development of cirrhosis caused by this viral infection.
- Routine liver function tests and monitoring can help detect the early signs of liver disease, allowing for timely intervention and prevention of cirrhosis.
Home Remedies for Liver Cirrhosis
Several home remedies and lifestyle modifications can complement the medicinal treatment plan and support overall liver health. These include:
- Dietary Changes: Adopting a balanced, nutrient-rich diet that is low in sodium and high in fibre can improve liver health and manage symptoms. Specific nutritional recommendations may include:
- Optimal intake of fruits, vegetables & whole grains
- Limiting consumption of red meat and processed foods
- Staying hydrated by drinking plenty of water
- Avoiding or limiting alcohol consumption
- Herbal Supplements: Supplements such as milk thistle, turmeric, and garlic have been recognised for their potential to support liver health and reduce inflammation. However, consulting with a doctor before starting any new supplements is crucial.
- Exercise: Regular, moderate physical activity can help improve liver function, reduce inflammation, and support overall well-being.
- Stress Management: Chronic stress can exacerbate liver disease, so incorporating stress-reducing techniques, such as meditation, deep breathing, or relaxation exercises, can be beneficial.
- Smoking Cessation: Quitting smoking can help prevent further liver damage and lower the risk of complications associated with cirrhosis.
Conclusion
Cirrhosis is a serious progressive liver disease that can significantly impact an individual's health and quality of life. By understanding the causes, symptoms, and treatment modalities for cirrhosis, individuals can take proactive steps to manage the condition and prevent further complications.
FAQS
1. How common is cirrhosis?
Cirrhosis is a relatively common liver disease affecting millions of people worldwide, alcohol-related cirrhosis & nonalcoholic fatty liver disease being the most prevalent
causes.
2. Can your liver recover from cirrhosis?
The liver can recover from the early stages of cirrhosis if the underlying cause is addressed and the progression of the disease is halted. However, advanced or end-stage cirrhosis is generally considered irreversible, and the focus shifts to managing the condition and preventing further complications.
3. Can cirrhosis be reversible?
While cirrhosis is often a progressive disease, in some cases, the liver can show signs of regeneration and improvement if the underlying cause is addressed promptly. It is more likely to occur in the early stages of the disease before extensive scarring has occurred. However, in advanced cases, the damage to the liver is typically irreversible.
4. What is a good diet for cirrhosis?
A balanced, nutrient-rich diet is essential for individuals with cirrhosis, including:
- Reduced sodium and limited consumption of red meat and processed foods
- Increased consumption of organic vegetables, fruits, and whole grains
- Lean protein sources, like fish, poultry, or plant-based options
- Proper hydration by drinking plenty of water
- Avoidance or limited consumption of alcohol

Still Have a Question?



