-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Cholera
Symptom, Causes, Diagnosis and Treatment
Cholera
Cholera remains one of the world's most serious bacterial infections, affecting millions of people globally each year. This potentially life-threatening disease can spread rapidly through communities, especially in areas with poor sanitation and limited access to clean water. This comprehensive guide explains cholera sickness, from its causes & symptoms to treatment modalities and prevention methods.
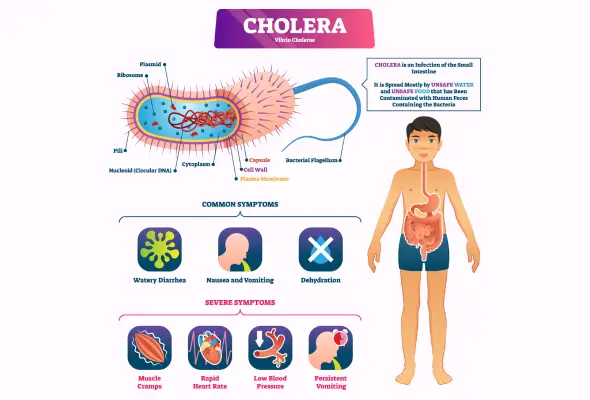
What is Cholera?
Cholera is an acute diarrhoeal infection when a person consumes food or water contaminated with the bacterium Vibrio cholerae. This severe bacterial disease produces a potent toxin in the small intestine that causes the body to release enormous amounts of water, leading to life-threatening dehydration.
Symptoms of Cholera Disease
The manifestation of cholera symptoms can vary significantly among infected individuals. While many people remain asymptomatic, they can still spread the bacteria through their stool for up to 14 days. When symptoms do appear, they develop within 12 hours to 5 days after exposure.
The following are the primary cholera virus symptoms:
- Watery diarrhoea with a pale, milky appearance (often called "rice water stools")
- Sudden vomiting that can last for hours
- Muscle cramps due to rapid loss of salts
- Extreme thirst and fatigue
- Fast heart rate and dizziness
Approximately 1 in 10 people develop severe symptoms that can become life-threatening. In these cases, diarrhoea can cause dangerous fluid loss of up to one quart per hour. Severe dehydration can occur within hours of symptom onset, leading to the loss of more than 10% of body weight.
Signs of severe dehydration include:
- Sunken eyes
- Dry mouth
- Shriveled skin that takes time to bounce back when pinched
- Minimal urination
Causes of Cholera
Cholera is caused by the Vibrio cholerae bacterium. The cholera spread is closely linked to environmental and social conditions. In regions affected by conflict, population displacement, and natural disasters, the risk of cholera outbreaks increases significantly due to compromised water and sanitation infrastructure.
Several factors can increase an individual's vulnerability to cholera infection. Poor sanitary conditions are the major risk factor, particularly in areas without proper water treatment facilities.
People may face a higher risk of severe cholera infection due to various personal factors:
- Blood Type O: Individuals with type O blood are twice as likely to develop severe cholera compared to other blood types
- Reduced Stomach Acid: People taking antacids or those with naturally low stomach acid levels face increased risk as the bacteria thrive in less acidic environments
- Dietary Choices: Consuming raw or undercooked shellfish, particularly from contaminated waters, significantly increases infection risk
- Living Conditions: Those residing in crowded areas with limited access to clean water & proper sanitation face elevated risk
- Medical Conditions: Individuals with long-standing medical conditions or those who have undergone gastrectomy are more susceptible
Complications of Cholera
The most severe complications of cholera include:
- Hypovolemic shock from severe dehydration
- Low blood sugar (hypoglycaemia) in children
- Potassium deficiency - affecting heart and nerve function
- Kidney failure accompanying shock
- Heart rhythm irregularities due to electrolyte imbalance
Diagnosis
The most definitive way to confirm cholera is by identifying Vibrio cholerae in a stool sample.
Doctors typically use several diagnostic approaches:
- Basic Laboratory Tests:
- Complete blood count
- Serum electrolytes
- Blood urea nitrogen
- Serum lactate levels
- Arterial blood gas analysis
- Rapid Diagnostic Tests (RDTs): RDTs have become valuable tools, especially in remote areas with poor laboratory facilities. These dipstick tests enable quick confirmation of cholera cases, helping to reduce mortality rates during outbreaks. However, while RDTs are helpful for early detection of probable cholera outbreaks, they should not be relied upon for routine diagnosis.
- Other Tests: The gold standard for diagnosis remains the culture-based method, specifically thiosulfate-citrate-bile salts-sucrose (TCBS) agar. Additionally, molecular detection methods, particularly Polymerase Chain Reaction (PCR), are gaining prominence in epidemic surveillance due to their better sensitivity and accuracy compared to traditional culture methods.
Treatment for Cholera
The cornerstone of cholera treatment is rehydration therapy, which has proven highly successful in preventing deaths. With proper treatment, the fatality rate drops to less than 1%.
The primary treatment options include:
- Oral Rehydration Solution (ORS): A mixture of salts and minerals that helps replace lost fluids
- Intravenous Fluids: Required for severely dehydrated patients
- Antibiotics: Used in severe cases to reduce symptoms
- Zinc Supplements: Specifically for children aged 6 months to 5 years
When to See a Doctor
Emergency warning signs requiring immediate medical attention include:
- Severe diarrhoea or vomiting
- Muscle cramps
- Extreme thirst
- Little to no urination
- Dizziness or weakness
- Rapid heart rate
- Confusion or altered mental state
For individuals living in or returning from areas with active cholera cases, any severe diarrhoea should be evaluated by doctors immediately. Even in regions where cholera is less common, severe dehydration can be a medical emergency that requires immediate care.
Cholera Prevention
The World Health Organisation emphasises that prevention is crucial in controlling cholera outbreaks and saving lives through improved sanitation & access to clean water.
Essential Prevention Measures:
- Use safe, treated water for drinking and food preparation
- Practice regular hand washing with soap & clean water
- Maintain proper toilet facilities and waste disposal
- Cook food thoroughly and avoid raw seafood
- Keep kitchen areas clean and sanitised
- Vaccination: These vaccines protect for at least three years with two doses, preventing approximately two out of three cholera infections.
Conclusion
Cholera remains a serious global health threat, but modern medicine offers practical solutions for prevention and treatment. Quick identification of symptoms and immediate medical care can reduce the death rate to less than 1%, making early action crucial for survival.
Simple preventive measures like clean water, proper sanitation, and good hygiene habits can protect communities from cholera outbreaks. Vaccines provide additional protection, though their availability varies by region. Healthcare systems worldwide continue to improve their response to outbreaks through better surveillance and treatment protocols.
People who live in or travel to high-risk areas should stay alert to cholera symptoms and seek medical help right away if they experience severe diarrhoea. Medical advances, combined with public health measures and community awareness, make cholera a preventable and treatable disease despite its dangerous nature.
FAQs
1. How can cholera spread?
Cholera spreads primarily through indirect contact when people consume contaminated water or food. The bacteria can contaminate water supplies and food preparation areas, particularly in regions with inadequate sanitation. People can contract cholera by:
- Drinking water contaminated with faeces containing V. cholerae
- Consuming raw shellfish from contaminated waters
- Eating food prepared with contaminated water
2. What are the three stages of cholera?
The progression of cholera follows three distinct stages:
- Stage of Inflammation: Initial bacterial infection and immune response
- Stage of Villus Fusing: Changes in intestinal structure
- Stage of Villus Resolution: Recovery phase of intestinal tissue
3. How is cholera cured?
Treatment focuses on replacing lost fluids & electrolytes. With proper treatment, the survival rate exceeds 99%. The primary treatment methods include:
- Oral rehydration solution (ORS)
- Intravenous fluids for severe cases
- Antibiotics like doxycycline or azithromycin
- Zinc supplementation for children
4. Does boiling water remove cholera?
Boiling may eliminate cholera bacteria from water. The CDC recommends heating water to a rolling boil for 1 minute to make it safe for consumption. Studies in Guatemala showed that boiling reduced bacterial contamination by 86.2%.
5. How long does cholera last?
The duration of cholera varies depending on treatment timing and severity. Most cases resolve within a few days to several weeks with proper treatment. Symptoms typically appear between 12 hours to 5 days after infection.
To Book an Appointment, call:
Still Have a Question?