-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Cardiomyopathy
Symptom, Causes, Diagnosis and Treatment
Cardiomyopathy
Did you know a healthy heart can pump about 2,000 gallons of blood daily? Cardiomyopathy, a group of ailments that affect the heart muscle, can severely impact this vital function. This condition causes a revolution in how the heart pumps blood throughout the body, leading to various health complications.
Cardiomyopathy is a serious heart disease that requires prompt attention and proper treatment to manage effectively. Understanding cardiomyopathy is crucial to tackle this challenging condition. Let's explore the different types of cardiomyopathy, its causes, and various cardiomyopathy symptoms. We'll also look into the risk factors, potential complications, and methods to diagnose this heart problem. Additionally, we'll discuss cardiomyopathy treatment options, prevention strategies, and when you should see a doctor. By the end, you'll have a better grasp of heart disease cardiomyopathy and how to manage it.
What is Cardiomyopathy?
Cardiomyopathy is a heart disease that affects the cardiac muscles, making it difficult for the heart to pump blood to the rest of the body. This condition causes the heart to lose its ability to function effectively, leading to various complications. In most cases, cardiomyopathy causes the heart muscles to become enlarged, thick, or rigid. As the disease advances, the heart becomes weaker and less capable to maintain a normal electrical rhythm.
The weakened heart can result in heart failure or irregular heartbeats called arrhythmias. People with cardiomyopathy may experience fatigue, shortness of breath, or heart palpitations. As the condition worsens over time, the heart can enlarge and weaken further, potentially leading to the need for a heart transplant in some cases.
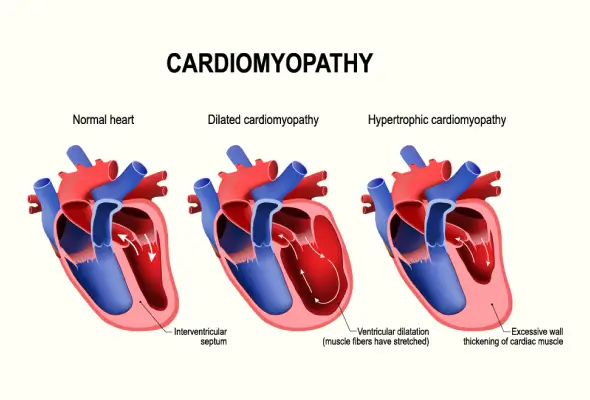
Types of Cardiomyopathy
Cardiomyopathy encompasses various forms of heart muscle disorders. The main kinds of cardiomyopathy include:
- Dilated Cardiomyopathy: This type is the most common cardiomyopathy, which causes the ventricles to weaken and enlarge, making it harder for the heart to pump blood effectively.
- Hypertrophic Cardiomyopathy: This cardiomyopathy type results in thickened heart muscle, particularly in the ventricles, which can obstruct blood flow.
- Restrictive Cardiomyopathy: It leads to stiffened ventricles, limiting their capability to relax and fill with blood.
- Arrhythmogenic Right Ventricular Cardiomyopathy: This cardiomyopathy type occurs when the muscle tissues in the right ventricle die, and scar tissue replaces it. This process disrupts the heart's electrical signals.
- Transthyretin Amyloid Cardiomyopathy: A rare form more common in African-American men.
- Stress Cardiomyopathy: Also called broken heart syndrome can occur following extreme emotional stress.
Causes of Cardiomyopathy
Cardiomyopathy can be inherited or acquired.
Inherited cardiomyopathy results from genetic mutations passed down from parents, affecting heart development. Hypertrophic and arrhythmogenic cardiomyopathies are often inherited.
Acquired cardiomyopathy develops due to other conditions or lifestyle factors. These include:
- Long-term high blood pressure
- Heart attacks
- Rapid heart rate
- Heart valve problems
- COVID-19 infection
- Metabolic disorders like obesity and diabetes
- Nutritional deficiencies
- Pregnancy complications
- Iron buildup in the heart muscle
- Sometimes, the cardiomyopathy cause remains unknown.
Symptoms of Cardiomyopathy
Cardiomyopathy symptoms can vary widely among individuals. Some people may not experience any signs, especially in the early stages of the disease. For others, symptoms appear as the condition worsens. Common signs include:
- Shortness of breath, particularly during physical activity or even at rest.
- Chest pain, especially after exertion or heavy meals
- A feeling of rapid, pounding, or fluttering heartbeats
- Swelling in the legs, ankles, feet, and neck veins
- Fatigue
- Dizziness and fainting
- Some individuals may have trouble lying flat to sleep or experience a cough while lying down.
It's important to note that symptoms worsen without treatment, and the progression rate can vary significantly between individuals.
Risk Factors
Cardiomyopathy can occur in people of all ages, races, and ethnicities. Certain factors increase the risk of this heart condition, such as:
- Age plays a role, with different types of cardiomyopathy more common in specific age groups.
- Excessive alcohol consumption
- Use of cocaine or amphetamines
- Exposure to very stressful situations
- Family history of heart conditions
- Certain medical treatments like chemotherapy or radiation for cancer
- Other medical conditions, including muscular dystrophy, sarcoidosis, heart inflammation, viral infections, obesity, diabetes, and thyroid disease, can contribute to the development of cardiomyopathy.
Complications of Cardiomyopathy
Cardiomyopathy can lead to serious health issues as the condition progresses.
- Heart failure, resulting in shortness of breath, tiredness, and fluid buildup in the body.
- Blood clots may form due to poor pumping, potentially causing strokes or pulmonary embolisms.
- Irregular heartbeats, or arrhythmias, can occur, sometimes leading to cardiac arrest.
- Heart valve problems may develop as the heart enlarges.
- In severe cases, cardiomyopathy can cause sudden death.
These cardiomyopathy complications can significantly impact the quality of life, making daily tasks challenging. The long-term outlook depends on factors such as the type of cardiomyopathy, response to treatment, and extent of heart damage.
Diagnosis of Cardiomyopathy
Diagnosing cardiomyopathy includes a combination of medical history, physical examination, and various tests. Doctors typically start by reviewing the patient's symptoms and family history of heart conditions.
- Physical Exam: Doctors listen to the heart and lungs using a stethoscope, checking for unusual sounds that might suggest cardiomyopathy.
- Blood Tests: Help identify infections or diseases that may lead to this heart condition.
- Electrocardiogram (ECG): An ECG detects abnormal rhythms, enlargement of the heart chambers, or signs of previous heart damage.
- Echocardiograms: Echocardiograms help create detailed images of the heart, showing its size, shape, and how well it's functioning.
- Chest X-rays: A chest X-ray checks for an enlarged heart or fluid buildup in the lungs.
- Stress Tests: A stress test measures how the heart works during physical activity and can help assess the severity of the condition.
- In some cases, more advanced procedures like cardiac catheterisation or genetic testing may be necessary to confirm the diagnosis.
Treatment for Cardiomyopathy
Cardiomyopathy treatment aims to manage symptoms, slow disease progression, and reduce complications. The approach depends on the type and severity of the condition.
- Lifestyle changes are crucial, including a heart-healthy diet, regular exercise, and avoiding alcohol and tobacco.
- Doctors may prescribe medications, such as antihypertensives, blood thinners, and antiarrhythmics, to improve blood flow and manage symptoms.
- Doctors may sometimes use devices like pacemakers or implantable cardioverter defibrillators to control irregular heart rhythms.
- For severe cases, doctors may perform procedures such as septal myectomy or alcohol septal ablation.
- In end-stage heart failure, a heart transplant may be necessary when other treatments have failed.
When to See a Doctor
- If you experience symptoms of cardiomyopathy, it's crucial to seek medical attention promptly.
- Contact your doctor if you notice shortness of breath, chest pain, or heart palpitations.
- Seek emergency care for severe chest pain, fainting, or worsening symptoms.
- If you have a family history of heart conditions, consider getting evaluated even without symptoms.
- Regular check-ups are essential for those diagnosed with cardiomyopathy to monitor their heart's health.
Preventions
While some forms of cardiomyopathy are inherited and cannot be prevented, there are steps to lower the risk of acquired cardiomyopathy, such as:
- Managing cholesterol levels and blood pressure is crucial.
- Regular workouts and maintaining a healthy weight can positively impact heart health.
- Avoiding tobacco products, limiting alcohol consumption, and steering clear of cocaine use are essential preventive measures.
- It's important to manage underlying conditions such as sleep apnea or diabetes.
- Early evaluation is recommended for those with a family history of heart conditions.
- Scheduling regular check-ups with a doctor and taking prescribed medicines as directed can help prevent complications.
Conclusion
Cardiomyopathy poses significant challenges to heart health, affecting people of all ages and backgrounds. This condition profoundly impacts the heart's ability to pump blood effectively, leading to various complications that can significantly impact quality of life. Understanding the different types, symptoms, and cardiomyopathy reasons is crucial to managing this heart condition effectively and improving outcomes for those affected.
By adopting a heart-healthy lifestyle, staying vigilant about symptoms, and seeking medical attention when needed, people can take proactive measures to support their heart health. Remember, while some forms of cardiomyopathy can't be prevented, many risk factors are within our control, making it possible to lower the chances of developing this serious heart condition.
FAQ's
1. What is the average age for cardiomyopathy?
The average age for diagnosing hypertrophic cardiomyopathy is around 39 years. However, cardiomyopathy can affect people of all ages, including children.
2. Is cardiomyopathy a disease of the cardiac muscle?
Yes, cardiomyopathy is a disease that affects the heart muscle. It causes the heart to lose its ability to pump blood effectively, leading to various complications.
3. What are the four signs of cardiomyopathy?
Four common signs of cardiomyopathy include shortness of breath, chest pain, heart palpitations, and swelling in the legs, ankles, or feet.
4. Is cardiomyopathy cured?
There's no cure for cardiomyopathy, but you can manage it. Many individuals can live normal, healthy lives with proper treatment and lifestyle changes.
5. Does ECG show cardiomyopathy?
An ECG can show signs that suggest cardiomyopathy, such as abnormal heart rhythms or changes in the heart's electrical activity. However, it's not definitive on its own.
6. How do you confirm cardiomyopathy?
Cardiomyopathy is confirmed through a combination of tests, including echocardiograms, cardiac MRI, blood tests, and sometimes a heart biopsy. A cardiologist typically makes the diagnosis after reviewing all test results.
Still Have a Question?