-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Bedsores
Symptom, Causes, Diagnosis and Treatment
Bedsores
Bedsores (pressure ulcers) affect millions worldwide, particularly those who remain restricted to beds or wheelchairs for extended periods. This comprehensive guide explains everything about bed sore treatment, from early warning signs to effective home care methods. You will learn about bedsore types, bed sore prevention techniques, proper wound care, and warning signs that require medical attention. The blog also covers different types of treatment for bedsores and when to seek professional help, making it an essential resource for caregivers and patients alike.
What are Bedsores?
Pressure ulcers, commonly known as bedsores, are areas of damaged skin & underlying tissue that develop when prolonged pressure reduces blood flow to specific body parts. These wounds can form in as little as two hours when constant pressure cuts off vital blood supply to skin cells, causing them to die.
Bedsores typically develop on parts of the body where bones are closest to the skin, including:
- Heels
- Ankles
- Elbows
- Shoulders
- Hips
- Tailbone
- Back
- Buttocks
- Back of the head
Causes and Risk Factors of Bedsores
The development of pressure ulcers stems from three primary mechanical forces that damage skin tissue. Understanding these forces and associated risk factors is crucial for prevention and treatment.
Primary Bedsore Causes
- Sustained Pressure: Constant force restricts blood flow to tissues
- Friction: Skin rubbing against bedding or clothing
- Shear Force: Skin moving in the opposite direction to underlying tissues
Several factors significantly increase the likelihood of developing bedsores:
- Medical Conditions
- Diabetes- affecting blood circulation
- Vascular diseases- limiting blood flow
- Spinal cord injuries- reducing sensation
- Neurological disorders- affecting mobility
- Physical Factors
- Age over 70 years
- Underweight condition
- Fragile or sensitive skin
- Poor nutrition and dehydration
- Incontinence issues
- Individuals in intensive care units
- Individuals recovering from recent surgery
- People with limited mobility, especially those confined to wheelchairs or beds
- Moisture from sweating or incontinence
- Poor nutrition, particularly inadequate protein, vitamin, and mineral intake
Symptoms
The initial symptoms vary and depend on skin tone and the stage of development. Early warning signs include:
- Skin discolouration (red on light skin, purple or blue on darker skin)
- Areas that feel warmer or cooler than the surrounding skin
- Patches that remain discoloured after pressure is removed
- Tender or painful spots
- Unusual firmness or sponginess of skin
- Itching or burning sensations
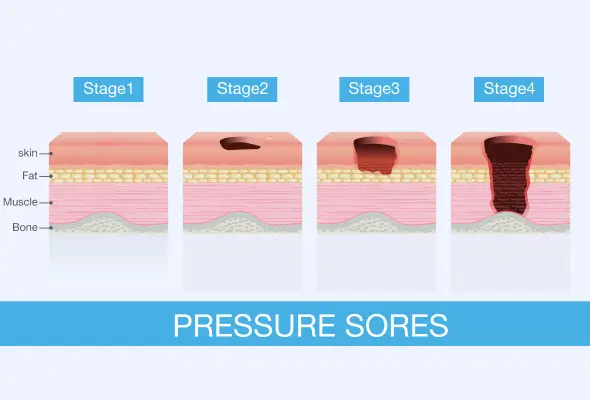
As pressure ulcers progress, they develop distinct characteristics at each bed sore stage:
- Initial Stage: Warm, discoloured patches that don't blanch when pressed
- Intermediate Stage: Shallow wounds or fluid-filled blisters
- Advanced Stage: Crater-like wounds with visible fatty tissues
- Severe Stage: Deep wounds with possible bone or muscle exposure
Warning Signs of Infection
These include:
- Drainage of pus
- Foul odour
- Increased pain around the affected area
- Fever, chills, or confusion if the infection spreads.
Complications
When bedsores advance beyond their initial stages, they pose significant risks to a patient's overall health and recovery.
Major complications of untreated bedsores include:
- Cellulitis (skin and soft tissue infection)
- Bone and joint infections
- Cancer development (Marjolin ulcer)
- Sepsis
- Life-threatening tissue damage
- Gangrene
- The most serious complication is septic shock, which occurs when infection spreads throughout the body via the bloodstream. This condition can become life-threatening and requires immediate medical intervention.
Diagnosis
Doctors use several validated risk assessment tools to evaluate patients:
- Norton Scale: Assesses the risk of pressure ulcers in adult patients. The scale comprises five items, including the patient's physical condition, mental state, activity, mobility, and incontinence.
- Waterlow Tool: This bedsore risk assessment tool comprises several components, such as build, skin type, mobility factors, age, and individual risk factors.
- Braden Tool: This tool predicts the risk of pressure ulcers in the patients. It comprises several subscales, including sensory perception, moisture, and activity levels.
During the diagnostic process, doctors typically conduct:
- Physical examination of the affected area
- Blood tests to assess overall health status
- Tissue cultures if infection is suspected
- Imaging tests like X-rays or MRIs when deeper tissue damage is possible
Based on the examination, doctors assign a stage to the pressure ulcer, which helps determine the most appropriate bedsore ulcer treatment plan. This staging process is crucial for monitoring the wound's progression and adjusting care strategies as needed.
Treatments for Bedsores
The treatment of pressure ulcers requires a comprehensive approach that combines proper wound care, pressure relief, and nutritional support.
Treatment approaches typically include:
- Effective Wound Care: Doctors recommend:
- Cleaning wounds with saline solution to remove dead tissue
- Applying appropriate dressings (films, gauzes, gels, or foams)
- Using specialised mattresses and cushions for pressure relief
- Changing position every 2-4 hours depending on risk level
- Professional Medical Care: It may include surgical debridement to remove dead tissue, specialised dressings, and advanced therapies. In severe cases, surgery might be necessary to add muscle flaps or skin grafts.
- Proper Nutrition: It plays a vital role in healing pressure ulcers. The body requires adequate calories, protein, vitamin C, and zinc to support tissue repair. Doctors might recommend supplements to promote faster healing.
- Regular Monitoring for Signs of Infection: Keep an eye on the signs of bedsore infection, which include foul odour or increased pain.
When to See a Doctor
Individuals should immediately contact their treating doctors if they notice:
- Hot, swollen, or red skin (appears purple or blue on darker skin)
- Pus discharge from the ulcer
- High temperature or fever
- Severe pain or worsening discomfort
- Changes in skin colour or texture
- Unusual tenderness or warmth around the affected area
Prevention
Essential preventive measures include regular position changes and proper skin care:
- Check skin daily for early warning signs
- Keep skin clean and moisturised
- Change position every 4-6 hours while in bed
- Shift weight every 15-20 minutes in a wheelchair
- Maintain good nutrition and hydration
- Use appropriate pressure-relieving equipment; proper equipment selection plays a crucial role in prevention. Doctors recommend specific support surfaces based on individual risk factors, such as foam mattresses, gel cushions, or air mattresses.
- Skin care guidelines should be followed meticulously. These are:
- Keep the skin clean & dry, particularly in areas prone to moisture.
- Apply moisturising creams daily.
- For individuals with incontinence, prompt cleaning and barrier creams help protect vulnerable areas.
- A balanced diet enriched in protein, vitamins & minerals helps maintain skin integrity.
- Wheelchair Precautions:
- For wheelchair users, proper sizing and cushioning are essential.
- Regular assessment of wheelchair fit and cushion condition helps prevent pressure points from developing.
- Specialised cushions should be checked daily for proper inflation and positioning.
Conclusion
Prevention remains the most effective strategy against bedsores through daily skin checks, proper positioning, and the use of pressure-relieving equipment. Regular monitoring helps catch early warning signs before they develop into serious complications. Caregivers and patients who understand the risks and follow proper care guidelines achieve better outcomes in managing pressure ulcers. The combination of vigilant prevention, proper treatment, and timely medical intervention helps ensure the best possible results for people at risk of developing bedsores.
FAQs
1. How can bed sores in older people be treated and managed?
Treatment for elderly patients requires special attention to skin sensitivity and overall health conditions. Doctors recommend regular position changes every 2-4 hours and proper skin care. Essential treatment steps include:
- Keeping the wound clean with saline solution
- Using prescribed dressings appropriate for the wound stage
- Ensuring proper nutrition with adequate protein intake
- Maintaining good skin moisture balance
2. Can bedsores be treated at home?
Home treatment is possible for early-stage pressure ulcers under a doctor's guidance. Proper wound cleaning, regular dressing changes, and careful monitoring form the foundation of home care. However, stage 3 and 4 bedsores require professional medical attention.
3. Is bedsore curable?
Most pressure ulcers heal with appropriate treatment, particularly those in stages 1 and 2. Recovery time varies and depends on the wound stage, overall health, and adherence to treatment protocols. Some severe cases may require surgical intervention for complete healing.
4. Is antibiotic cream good for bedsores?
Antibiotic creams can be beneficial when doctors prescribe for infected pressure ulcers. However, not all bedsores require antibiotic treatment. Doctors determine the need based on wound assessment and signs of infection.
5. What are the Common sites of pressure ulcers?
Common pressure points vary based on body position and mobility, such as:
- Lying Position: Heels, tailbone, shoulders
- Sitting: Buttocks, spine, shoulder blades
- Side-lying: Hips, ankles, ears
To Book an Appointment, call:
Still Have a Question?