-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Astrocytoma
Symptom, Causes, Diagnosis and Treatment
Astrocytoma
Astrocytoma affects thousands of lives each year as one of the most common types of brain tumours. This condition develops in the brain's astrocytes, the star-shaped cells that protect nerve tissue and help maintain the blood-brain barrier. This comprehensive guide explores astrocytoma brain tumour symptoms, causes, diagnosis methods, and current treatment approaches available to patients.
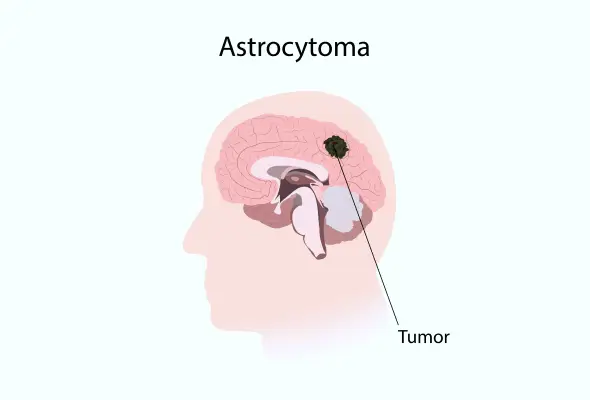
What is Astrocytoma?
The central nervous system houses a specific type of tumour called astrocytoma, which develops from star-shaped cells known as astrocytes. These specialised cells play an elementary role in supporting and connecting nerve cells within the brain and spinal cord. Astrocytoma is the most prevalent form of glioma, constituting 60% of all brain tumours.
These tumours can develop with varying levels of severity, ranging from slow-growing benign masses to aggressive cancerous growths. Key characteristics of astrocytoma include:
- Location: Primarily develops in the brain but can also affect the spinal cord
- Growth patterns: Can be slow-growing (benign) or fast-growing (malignant)
- Age variation: Different grades affect various age groups differently
- Impact: This can cause both physical and neurological symptoms depending on location. Astrocytoma in the spine can cause pain, weakness, and mobility issues
- Treatment approach: Varies based on tumour grade and location
Types of Astrocytoma
The World Health Organisation (WHO) marks astrocytomas into four grades, ranging from slow-growing tumours to highly aggressive forms.
Non-cancerous Astrocytomas (Grade 1): These slow-growing tumours include:
- Pilocytic Astrocytoma: The most common Grade 1 type, typically developing in the cerebellum
- Pleomorphic Xanthoastrocytoma: Usually affects the temporal lobe and often causes seizures
- Subependymal Giant Cell Astrocytoma: Primarily occurs in children with tuberous sclerosis
Cancerous Astrocytomas: Grade 2 through 4 astrocytomas are considered cancerous, with increasing levels of aggression:
- Grade 2 (Diffuse Astrocytoma): These tumours tend to infiltrate nearby brain tissue
- Grade 3 (Anaplastic Astrocytoma): More aggressive than Grade 2, these tumours often develop as a progression from lower grades and require comprehensive treatment, including radiation and chemotherapy
- Grade 4 (Glioblastoma): The most aggressive form, making up more than 50% of all astrocytomas. In 90% of cases, these tumours begin as Grade 4, while 10% develop from lower-grade tumours.
Symptoms of Astrocytoma
The manifestation of astrocytoma symptoms depends significantly on the tumour's grade and location within the brain or spinal cord.
- Common Physical Symptoms:
- Persistent headaches that may differ from typical headaches
- Nausea & vomiting due to increased intracranial pressure
- Vision changes, including double vision or blurriness
- Persistent back or limb pain
- Balance and coordination difficulties
- Fatigue and general weakness
- Neurological and Cognitive Changes:
- Seizures or focal seizures
- Memory loss and confusion
- Personality changes and mood alterations
- Speech difficulties (aphasia)
- Depression
Causes and Risk Factors of Astrocytoma
While the exact cause remains undetectable in most cases, scientists have identified several key risk factors that may contribute to tumour formation.
- Radiation Exposure: Exposure to ionising radiation significantly increases the risk of developing astrocytoma. Children who receive preventive radiation therapy for acute lymphocytic leukaemia face a 22 times higher risk of developing central nervous system tumours within 5 to 10 years. Similarly, patients receiving pituitary adenoma radiation therapy show a 16 times greater risk of glioma development.
- Genetic Factors: Several inherited conditions can increase the likelihood of developing astrocytoma:
- Li-Fraumeni Syndrome - Caused by changes in the TP53 gene, resulting in a 90% lifetime cancer risk
- Neurofibromatosis Type 1 (NF1) - Leads to abnormal cell growth and early-onset astrocytomas
- Tuberous Sclerosis - Associated with specific types of astrocytomas due to TSC1 and TSC2 gene mutations
- Turcot Syndrome - Characterised by intestinal polyps and brain tumours
Complications of Astrocytoma
- Physical Complications: They are among the most common challenges, particularly affecting motor functions. Studies indicate that motor complications primarily impact fine motor skills. Additionally, patients may experience:
- Changes in physical appearance
- Pain in affected areas
- Fatigue and weakness
- Motor functioning difficulties
- Mobility issues
- Communication challenges
- Spinal deformities
- Loss of bladder or bowel movements
- Cognitive Complications: The cognitive impact of astrocytoma can be substantial, with research showing that patients often experience cognitive difficulties affecting their performance in school and daily life.
- Treatment-related Complications:
- Neurosurgical interventions may lead to infection, bleeding, and neurological deficits.
- Radiation therapy & chemotherapy can cause adverse effects such as fatigue, nausea, and cognitive decline.
Diagnosis
- Neurological Assessment: The diagnostic process begins with a detailed neurological examination, where doctors evaluate vision, hearing, balance, coordination, strength, and reflexes to identify affected brain areas.
- Imaging: Advanced imaging techniques form the cornerstone of diagnosis. Magnetic Resonance Imaging (MRI) stands as the gold standard, offering remarkable accuracy with 82-100% sensitivity rates and specificity of 81-100%. Healthcare teams employ several specialised imaging methods:
- Magnetic Resonance Spectroscopy (MRS)
- Perfusion-weighted imaging
- Functional MRI
- Computed Tomography (CT)
- Positron Emission Tomography (PET)
- Biopsy: The definitive diagnosis comes through a tissue biopsy, typically performed during surgery or through a needle procedure. This crucial step allows specialists to examine the tumour cells microscopically and perform molecular testing.
Astrocytoma Treatment
Surgery serves as the primary treatment option, providing three crucial benefits. It allows healthcare teams to obtain tissue samples for diagnosis, enables testing for specific protein mutations that certain medications could target, and helps remove as much of the tumour as possible. For grade 1 astrocytomas, surgery alone can often lead to a cure if the neurosurgeon can safely remove the entire tumour.
Following surgery, patients typically receive a combination of treatments:
- Radiation Therapy: This treatment uses external beam radiation therapy to target the remaining cancer cells. Doctors usually begin radiotherapy 2-4 weeks post-surgery.
- Chemotherapy: Temozolomide, taken daily for six weeks during radiation therapy, serves as the primary chemotherapy drug
- Tumor-treating Fields: A specialised device producing electrical fields to delay tumour growth, particularly useful for glioblastomas
For high-grade astrocytomas, treatment typically involves a comprehensive approach combining surgery, radiation therapy & chemotherapy to eliminate remaining cancer cells. The treatment cycle for chemotherapy usually spans several months, with medication taken for five days every four weeks.
When to See a Doctor
Immediate medical attention is necessary when:
- Memory problems develop or worsen
- Seizures occur
- Severe headaches or vision problems emerge
- Unexplained weight loss appears
- Loss of bladder or bowel functions
Prevention
While specific prevention methods remain elusive, research suggests that certain lifestyle modifications may help support overall health during and after treatment:
- Maintaining a balanced diet to support energy levels and recovery
- Staying well-hydrated before, during, and after treatments
- Monitoring protein, iron, vitamin B12, and calcium intake, especially for vegetarians
- Avoiding foods with high food poisoning risk during chemotherapy
- Following dietary restrictions as recommended by doctors
- Minimising exposure to ionising radiation when possible represents one of the few preventive measures current research supports.
Conclusion
Astrocytoma remains a complex condition that affects thousands of people each year. Though doctors cannot prevent astrocytoma, early detection and proper treatment significantly improve patient outcomes.
Research continues to advance treatment methods, giving hope to patients and their families. The combination of surgery, radiation therapy, and chemotherapy provides effective treatment paths for many patients. Regular medical check-ups and prompt attention to warning signs help doctors catch and treat astrocytoma early, leading to better results.
FAQs
1. Is there a cure for astrocytoma?
The possibility of a cure depends mainly on the tumour's grade. Surgery can cure most grade 1 astrocytomas if the neurosurgeon can safely remove the entire tumour. Very rarely, some grade 2 astrocytomas may also be curable through surgery. A combination of various treatments can help slow grade 3 and grade 4 astrocytoma growth and manage symptoms.
2. What are the first symptoms of astrocytoma?
Early warning signs of astrocytoma often include persistent and unexplained headaches that differ from typical headaches. Common initial symptoms include:
- Headaches that worsen in the morning
- Nausea and vomiting
- Changes in vision or speech
- Memory problems and confusion
- Seizures in about 50% of cases
3. What is the difference between glioblastoma and astrocytoma?
Glioblastoma represents a specific type of grade 4 astrocytoma, distinguished by its molecular profile. The key difference lies in their IDH enzyme status - astrocytomas are IDH-mutant tumours, while glioblastomas are IDH-wild-type. This distinction affects both treatment approaches and prognosis.
4. Can astrocytoma be removed entirely?
Complete removal depends on the tumour's location and grade. For grade 1 astrocytomas, complete surgical removal is often possible and can lead to a cure. However, higher-grade astrocytomas typically infiltrate surrounding brain tissue, making complete removal challenging or impossible.
5. How fast does astrocytoma grow?
Growth rates vary significantly based on the tumour's grade. Grade 1 and 2 astrocytomas are slow-growing, while grade 3 and 4 tumours grow rapidly and aggressively. The growth rate influences treatment decisions and prognosis, with higher-grade tumours requiring more aggressive treatment approaches.
To Book an Appointment, call:
Still Have a Question?