-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Ascites
Symptom, Causes, Diagnosis and Treatment
Ascites
Ascites is a medical condition that occurs when excess fluid builds up in the abdomen, causing potential health complications. Understanding ascites, their causes, and available treatments is crucial for those affected by this condition.
Ascites can stem from various underlying health issues, with liver disease being a common culprit. The symptoms of ascites can vary from mild discomfort to severe pain and breathing difficulties. This article will explore the causes of ascites, its symptoms and how doctors diagnose & treat this condition.
What is Ascites?
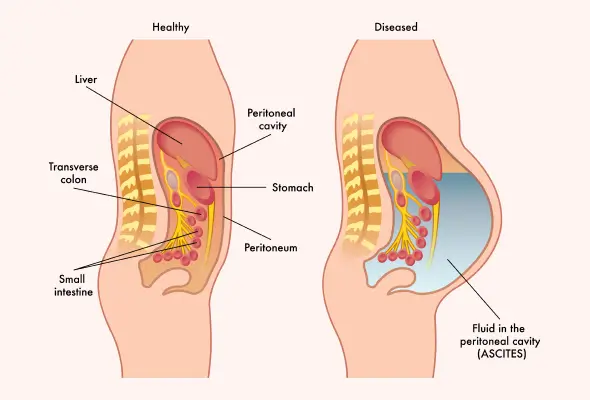
Ascites is a condition characterised by excessive accumulation of fluid in the abdomen. This accumulation occurs between the two layers of the peritoneum, a tissue sheet covering the abdominal organs. The condition often develops in individuals with cirrhosis, which is scarring of the liver. As fluid accumulates, it can cause the belly to swell, leading to discomfort and a range of symptoms. These may include abdominal pain, bloating, constipation, and shortness of breath. Ascites can result from increased pressure in the portal vein (This vein runs from the digestive organs to the liver). This rise in pressure can impair kidney and liver function, causing fluid to accumulate. While ascites itself is not typically life-threatening, it may indicate a more serious underlying condition.
Stages of Ascites
Ascites have a significant impact on liver cirrhosis patients, with approximately 60% developing this condition within a decade. The classification of ascites is based on the amount of fluid in the abdominal cavity.
- Grade 1: Mild ascites, which are detectable only by ultrasound examination.
- Grade 2: Moderate ascites, causes mild symmetrical abdominal distension.
- Grade 3: Large ascites, which results in significant abdominal distension.
The emergence of ascites marks a poor prognosis, with a mortality rate of about 40% after one year. Patients with uncomplicated ascites have an 85% one-year survival probability. However, this drops significantly for those with complications like hyponatremia, refractory ascites, or hepatorenal syndrome.
Causes of Ascites
Ascites have various causes, such as:
- Cirrhosis of the liver is the most common.
- Other Abdominal tuberculosis.
- Cancer in the abdomen, such as ovarian, pancreatic, or liver cancer, can also lead to ascites.
- Heart conditions, particularly congestive heart failure, may cause fluid build-up in the abdomen.
- Kidney diseases, infections, renal dialysis, and low protein levels can contribute to ascites development.
- Portal vein thrombosis, which involves blood clots in the liver's veins, and pancreatitis are other potential causes.
Understanding these causes is crucial for effective ascites treatment and managing underlying conditions.
Symptoms of Ascites
Ascites symptoms can develop gradually or suddenly, depending on the underlying cause. The main signs include abdominal distention and rapid weight gain. Individuals may develop abdominal pain, bloating, and discomfort as fluid accumulates. A large quantity of fluid accumulation can lead to shortness of breath as the diaphragm gets pushed upwards, compressing the lower lungs. Other symptoms include:
- Swelling in the ankles
- Digestive issues like loss of appetite and constipation
- Back pain
- Fatigue.
- Sometimes, spontaneous bacterial peritonitis may occur, causing fever, nausea, and abdominal tenderness.
The severity of symptoms often correlates with the amount of fluid in the abdominal cavity.
Diagnosis of Ascites
Doctors employ various methods to diagnose ascites.
- Physical Examination: A doctor will check for shifting dullness or bulging flanks, which can help identify ascites.
- Blood Tests: Doctors may conduct various blood investigations (liver function tests (LFT), renal function tests (RFT)) and infections & cancer markers to diagnose ascites.
- Abdominal Ultrasonography: It can detect even small amounts of fluid.
- Imaging Tests: In some cases, doctors perform computed tomography, laparoscopy, or MRI for a definitive diagnosis, especially if malignancy is suspected.
- Diagnostic Paracentesis: This procedure is considered the gold standard diagnostic test, in which doctors will extract a sample of ascitic fluid. This fluid is analysed for cell count, albumin levels, and culture to determine the cause. The serum-ascites albumin gradient (SAAG) is a crucial test, with a level of 1.1 g/dL or greater indicating portal hypertension.
Treatment of Ascites
The treatment of ascites typically involves a combination of approaches:
- Medications: Diuretics are the mainstay of therapy. Doctors sometimes prescribe antibiotics if the cause of ascites is infection.
- Low-sodium Diet: Dietary salt restriction to about 90 mmol/day is recommended.
- Paracentesis: Doctors often employ therapeutic paracentesis for patients with large or refractory ascites. This procedure involves draining ascitic fluid with volume expansion using albumin if more than 5 litres are removed.
- Shunt Placement: Sometimes, doctors suggest a transjugular intrahepatic portosystemic shunt (TIPS) placement for patients requiring frequent paracentesis.
Complications
Ascites can lead to serious complications if left untreated, including:
- Infection: One of the most common is spontaneous bacterial peritonitis, an ascitic fluid infection. This condition causes fever and abdominal pain, requiring immediate medical attention and antibiotic treatment.
- Hepatic Hydrothorax: In this condition, fluid accumulates in the lungs, causing breathing difficulties and chest discomfort.
- Hernia: The increased abdominal pressure from ascites can result in hernias, particularly umbilical and inguinal types.
- Kidney Impairment: Kidney failure, known as hepatorenal syndrome, may occur if cirrhosis worsens.
When to See a Doctor
If you have ascites, seeking medical attention is crucial if certain symptoms arise. Contact your doctor immediately if you experience:
- Fever above 38.05°C
- Abdominal pain
- Blood in your stool or vomit
- Easy bruising or bleeding
- Swollen legs or ankles
- Breathing problems
- Mental symptoms, such as confusion
- Yellowish discolouration in your skin and eyes (jaundice)
- Sudden weight gain, significantly more than 10 pounds or two pounds daily for three consecutive days.
Prevention
To prevent ascites or manage its progression, individuals can make several lifestyle changes:
- Abstaining from alcohol is paramount, as it can damage the liver and increase cirrhosis risk.
- Limiting salt intake to 2,000-4,000 mg daily helps reduce fluid retention.
- A healthy weight is essential, as obesity is a risk factor for ascites.
- Regular weight checks are essential; notify your doctor if you gain more than 5 kgs or 0.9 kg daily for three consecutive days.
- A balanced diet, regular exercise & avoiding tobacco contribute to overall health.
- Practising safe sex reduces the risk of hepatitis, which can lead to liver damage and ascites.
- Limited use of nonsteroidal anti-inflammatory drugs (NSAIDs) is also advisable, as they can affect kidney function and fluid retention.
Conclusion
Ascites profoundly impact those affected, with their various causes and symptoms presenting significant challenges for patients and doctors alike. From liver cirrhosis to heart conditions, the underlying issues leading to ascites require careful management and treatment. Prompt diagnosis and appropriate interventions are crucial to prevent complications and improve quality of life. This condition influences not only physical health but also emotional well-being, emphasising the need for comprehensive care.
The combination of medical therapies, lifestyle changes, and preventive measures offers hope for better management of this condition. Early detection & timely medical attention are key to addressing ascites and its potential complications.
FAQ's
1. Can ascites be cured?
Ascites can be managed effectively, but a complete cure depends on treating the underlying cause. In cases of alcohol-associated hepatitis, ascites may resolve with improvements in liver function. For patients with cirrhosis, treatments like diuretics, paracentesis, or TIPS can help control ascites. However, liver transplantation is often the only curative option for severe cases.
2. Should I drink a lot of water with ascites?
Fluid intake for ascites patients should be carefully managed. While excessive fluid restriction is generally not recommended, patients with severe hyponatremia may need to limit their water intake. Following your doctor's advice regarding fluid consumption is crucial, as individual needs may vary based on the severity of ascites and other complications.
3. Can ascites be removed?
Yes, paracentesis procedure can drain ascites. A needle is inserted into the abdomen to drain excess fluid during this process. For large-volume paracentesis, albumin infusion may be necessary to prevent complications. While this procedure provides temporary relief, it doesn't address the underlying cause of ascites, and the fluid may reaccumulate without further treatment.
4. How to check for ascites?
The diagnosis of ascites typically includes physical examination, imaging tests, and fluid analysis. Your doctor may check for signs like abdominal distension or shifting dullness. Abdominal ultrasound confirms the presence of fluid. In some cases, doctors may perform a diagnostic paracentesis to analyse the ascitic fluid and determine its cause.
5. Which food is best for ascites?
For patients with ascites, a low-sodium diet is beneficial. Recommended sodium intake is typically less than 2,000 to 4,000 milligrams per day. A dietitian can help create a suitable meal plan. Foods low in sodium, such as fresh fruits, vegetables, and lean proteins, are generally recommended.
6. What is the recovery time for ascites?
The recovery time for ascites varies and depends on the underlying cause and treatment approach. With appropriate management, some patients may see improvement within weeks. However, for those with chronic liver disease, managing ascites may be an ongoing process.
7. Can ascites come back?
Yes, ascites can recur, especially if the underlying cause persists. After successful treatment, the fluid may reaccumulate if liver function doesn't improve or patients don't adhere to dietary restrictions and medications. Regular follow-ups with doctors are essential to monitor for recurrence and adjust treatment as needed. In some cases, repeated paracentesis or consideration of other treatments like TIPS may be necessary.
To Book an Appointment, call:
Still Have a Question?




