-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Aortic Stenosis
Symptom, Causes, Diagnosis and Treatment
Aortic Stenosis
Aortic stenosis affects millions of people worldwide. This heart condition develops when the aortic valve narrows, making it harder for the heart to pump blood to the rest of the body. Aortic stenosis can significantly affect a person's quality of life and health. Understanding this heart condition is crucial for early detection and proper treatment. Let's understand what aortic stenosis is, the different types of it, and what causes it.
What is Aortic Stenosis Disease?
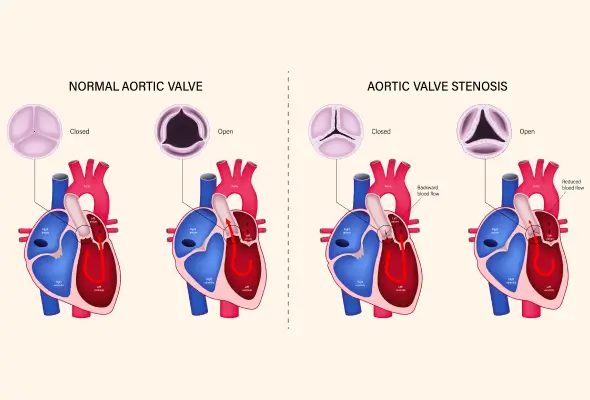
Aortic stenosis is a serious heart valve condition that occurs when the aortic valve, one of four valves in the heart, becomes narrowed or blocked. This narrowing restricts blood flow from the left ventricle to the aorta, making it harder for the heart to pump enough blood to the other body organs. As a result, it can limit the amount of oxygen reaching vital organs and tissues.
The aortic valve usually has three flaps (leaflets) that open to allow blood through and then close to prevent backflow. These leaflets may become stiff, thickened, or fused in aortic stenosis, hindering their proper function. This condition can cause various signs and symptoms, including palpitations, chest pain, breathlessness, and fainting. If left untreated, aortic stenosis can cause heart damage and even be life-threatening.
Types of Aortic Stenosis
Aortic stenosis can be classified into different types based on its origin and characteristics. The most common types are:
- Congenital aortic stenosis occurs when the aortic valve doesn't form properly during foetal development. It can present as unicuspid, bicuspid, tricuspid, or quadricuspid valves. The most common congenital aortic stenosis is bicuspid aortic valve stenosis, affecting about 2% of the population.
- Acquired aortic stenosis, on the other hand, develops over time and is more frequently encountered. It results from narrowing the aortic valve opening due to various factors, such as calcification or rheumatic heart disease.
- Understanding these types helps doctors determine the most appropriate treatment approach for patients with aortic stenosis.
Causes of Aortic Stenosis
Aortic stenosis has several causes, such as:
- Ageing: As people age, their aortic valves become calcified. This process makes the valve stiff and narrow.
- Birth Defects: Congenital heart defects, such as a bicuspid aortic valve, can also lead to aortic stenosis. In poor and developing countries, rheumatic heart disease is a major cause.
- Infections: When bacteria from untreated infections, such as scarlet fever and strep throat, reach blood circulation, they can build up on the heart valves and damage them.
- Other Causes: Other factors that contribute to aortic stenosis include high blood pressure, abnormal lipid levels, diabetes, and chronic kidney disease.
Aortic Stenosis Symptoms
Aortic stenosis often develops gradually; some people may not notice symptoms for years. However, as the condition progresses, various signs may appear. Common symptoms include:
- Chest pain or tightness
- Shortness of breath (particularly during physical activity or when lying down)
- Fatigue that disrupts normal activities
- Dizziness
- Lightheadedness or even fainting
- Heart palpitations and a rapid, fluttering heartbeat
- Individuals notice a decline in their ability to perform routine physical activities.
- Swelling in the ankles, feet, and the lower leg
Risk Factors
Several factors increase the risk of developing aortic stenosis, such as:
- Genetic predisposition may also play a part in some individuals.
- The condition is more common in people over 65. The prevalence of calcific aortic sclerosis, a precursor to aortic stenosis, ranges from 9% to 45% in patients aged 54 to 81.
- Men are more susceptible.
- High blood pressure
- Obesity, particularly abdominal fat distribution
- Smoking
- Abnormal lipid levels
- Diabetes
- Chronic kidney disease
Complications of Aortic Stenosis
Aortic stenosis can lead to serious complications if left untreated, such as:
- Heart failure is a common complication, as the heart struggles to pump blood effectively.
- The condition can cause thickening and stiffening of the heart muscle, leading to chest discomfort.
- Pulmonary hypertension can occur due to increased pressure in the left ventricle.
- In advanced stages, patients may experience frequent fainting spells or loss of consciousness.
- Some patients may also be at risk of cerebral or systemic emboli from calcific deposits on the valve.
- Sudden death is a risk, especially in patients with severe symptoms.
- Other potential complications include conduction abnormalities, increased risk of infective endocarditis, and bleeding problems.
Diagnosis of Aortic Stenosis
Diagnosing aortic stenosis involves a combination of physical examination and various diagnostic tests.
- Physical Examination: Doctors look for typical symptoms of aortic stenosis, like swelling in your lower legs and feet. Using a stethoscope, they may also hear the heart murmur, the telltale sign of aortic stenosis.
- Echocardiography: The primary tool for confirming aortic stenosis is echocardiography, which helps assess valve morphology, opening movement, and wall thickness.
- Electrocardiogram (ECG or EKG): This test measures the heart's electrical activity.
- Doppler Test: Doppler measurements help quantify the severity of aortic stenosis by measuring peak transvalvular velocity, mean pressure gradient, and aortic valve area.
- Imaging Tests: Angiography, cardiac computerised tomography (CT) scans and cardiac MRIs provide a detailed picture of the heart and valvular structures.
- Catheterisation: In some cases, cardiac catheterisation may be necessary for a definitive diagnosis.
Treatment for Aortic Stenosis
The aortic stenosis treatment approach depends on the presence of symptoms and the severity of the condition.
- Monitoring: Regular check-ups and lifestyle changes may be sufficient for mild cases. However, as the disease progresses, more aggressive interventions become necessary.
- Medical Treatment of Aortic Stenosis: Doctors prescribe various medicines to manage and treat heart rhythm disorders, high blood pressure or heart failure.
- Surgical Intervention: The main treatment options include valve repair and replacement.
- Balloon valvuloplasty, a minimally invasive procedure, can widen the narrowed valve, providing temporary relief.
- For more severe cases, doctors suggest a valve replacement procedure. This can be conducted through traditional open-heart surgery or using newer, less invasive techniques like transcatheter aortic valve replacement (TAVR).
When to See a Doctor
If you suspect you have aortic stenosis, it's crucial to consult a healthcare provider promptly. Seek medical attention if you experience symptoms like chest pain or tightness, palpitations, shortness of breath, or fainting spells. If you're considering pregnancy and have aortic stenosis, it's vital to discuss this with your doctor beforehand. For those already diagnosed, contact your doctor immediately if you notice new or worsening symptoms, such as increased fatigue, swollen ankles, or difficulty sleeping.
Preventions
While you cannot wholly prevent aortic stenosis, certain lifestyle changes can help maintain heart health and potentially slow its progression, such as:
- Eating a heart-friendly diet rich in fruits, vegetables, and whole grains while limiting excess salt and saturated fats is crucial.
- Regular exercise, such as brisk walking for 30 minutes daily, can help manage weight and control risk factors.
- Quitting smoking and managing stress through yoga, mindfulness, or support groups are also beneficial.
- It's important to control other cardiovascular conditions like hypertension and high blood cholesterol levels.
- Regular dental care is essential, as there's a link between gum disease and heart inflammation.
- Annual health check-ups can help detect early signs of aortic stenosis or other heart valve diseases.
Conclusion
Aortic stenosis is a serious cardiovascular condition that affects millions worldwide. It occurs when the aortic valve narrows, making it harder for the heart to pump blood effectively. Understanding aortic stenosis is crucial for early detection and proper management. While it can't be prevented entirely, adopting a heart-healthy lifestyle can help maintain cardiovascular health. If you experience symptoms like shortness of breath, chest pain, or fainting, see a doctor promptly. With proper care and treatment, many people with aortic stenosis can lead full and active lives.
FAQ's
1. How common is aortic stenosis?
Aortic stenosis becomes more prevalent with age. It affects about 5% of people at age 65, with an increasing prevalence in older age groups. In those aged 75 and above, the prevalence rises to 12.4%, with severe aortic stenosis present in 3.4% of this age group.
2. Is surgery the only option for aortic stenosis?
Surgery is not always the only option for aortic stenosis. Treatment strategy generally depends on the presence of symptoms and the severity of the condition. For mild cases, regular check-ups and lifestyle changes may be sufficient. Medications can help manage symptoms, but they cannot cure the condition. In more severe cases, valve repair or replacement may be necessary.
3. Can you recover from aortic stenosis?
Recovery from aortic stenosis depends on the treatment method. Surgical methods typically have longer recovery times than transcatheter methods like balloon valvuloplasty and TAVR. With timely or early treatment, the outlook for aortic stenosis is generally good to excellent.
4. Is walking good for aortic stenosis?
Regular physical activity, including walking, can benefit people with aortic stenosis. However, doctors should tailor the activity level to the individual's condition. Doctors often recommend regular exercises for those with mild aortic stenosis or no symptoms. Patients with moderate aortic stenosis may need to limit their activity. Always consult a doctor for personalised advice.
5. What are the best foods for aortic stenosis?
While there's no specific diet proven to prevent or treat aortic stenosis, doctors generally recommend a heart-healthy diet plan. This plan includes eating foods low in salt and fat and rich in fruits, vegetables, and whole grains. Regular physical activity and a balanced meal plan can help manage risk factors associated with aortic stenosis.
6. At what age do people get aortic stenosis?
Aortic stenosis can occur at any age, but it's most common in older adults. It's relatively uncommon in those under 65 years old unless there's a congenital abnormality. The risk increases significantly with age, with a notable rise in prevalence after 65 years. Aortic stenosis is often due to bicuspid aortic valve disease in younger age groups.

Still Have a Question?