-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Allergic Rhinitis
Symptom, Causes, Diagnosis and Treatment
Allergic Rhinitis
Allergic rhinitis is a common medical ailment affecting millions worldwide. It characterizes a runny nose, sneezing, and itchy eyes and can significantly impact daily life, causing discomfort and interfering with work, sleep, and leisure activities. This blog explores the causes, symptoms, and various allergic rhinitis treatment options.
What is Allergic Rhinitis?
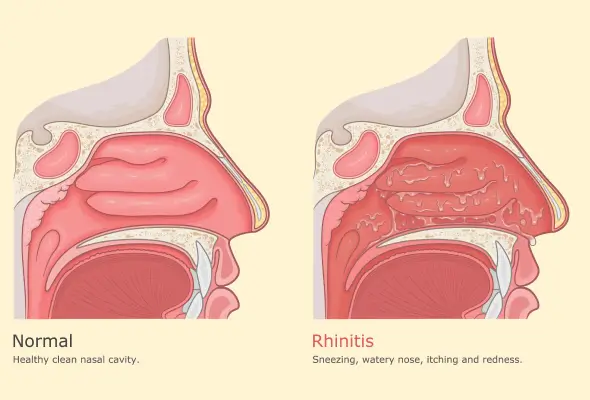
Allergic rhinitis, commonly called hay fever, is an allergic reaction, These allergies are due to tiny particles in the air called allergens. When people breathe in these allergens through their nose or mouth, their body releases a natural chemical called histamine. This reaction causes a group of symptoms affecting the nose, including sneezing, nasal congestion, clear rhinorrhea (runny nose), and nasal pruritis (itching).
Symptoms of Allergic Rhinitis
The allergic rhinitis symptoms typically appear quickly after exposure to allergens and can persist as long as the person remains in contact with them.
The following are some of the most common symptoms of hay fever:
- Nasal Issues:
- Runny nose with thin, watery discharge
- Nasal congestion (stuffiness)
- Sneezing
- Itchy nose
- Eye Problems:
- Red, watery eyes
- Itchy eyes
- Swollen, bruised-appearing skin under the eyes (allergic shiners)
- Throat and Mouth Discomfort:
- Itchy throat and roof of mouth
- Sore throat due to postnasal drip (mucus running down the back of the throat)
- Respiratory Symptoms:
- Coughing
- Wheezing
- Difficulty breathing
- Other Symptoms:
- Headaches and sinus pressure
- Extreme tiredness (fatigue), often due to poor sleep
Causes of Allergic Rhinitis (Hay Fever)
Allergic rhinitis develops when the immune system overreacts to harmless airborne substances called allergens. This triggers an immune response, causing the release of natural chemicals, primarily histamine, into the bloodstream.
This histamine release leads to inflammation of the mucous membranes in the eyes, nose & throat, resulting in the characteristic symptoms of allergic rhinitis, such as sneezing, runny nose, and itchy eyes.
Several indoor and outdoor allergens can cause hay fever. Common triggers include:
- Pollen from trees, weeds, and plants
- Mould spores
- Pet dander
- Dust mites
- Cockroach droppings and saliva
- Seasonal variations
Risk Factors for Hay Fever
Several factors can increase an individual's risk of developing allergic rhinitis. The following are some risk factors for hay fever:
- People with a blood relative, such as a parent or sibling, who has allergies or asthma are more susceptible
- Individuals with asthma or atopic dermatitis (eczema)
- Living or working in an environment with constant exposure to allergens
- Children whose mothers smoked during their first year of life have an increased risk of developing hay fever
- The "hygiene hypothesis" suggests that lowering the exposure to microbes during early childhood may contribute to the development of allergic diseases, including hay fever.
Diagnosis
Diagnosing allergic rhinitis involves a comprehensive approach to identifying the specific allergens causing the symptoms, including:
- The doctor starts with a physical examination and a detailed discussion of the patient's health, symptoms, and potential triggers.
- To confirm the diagnosis and arrive at the exact allergens responsible, doctors may recommend one or both of the following tests:
- Skin Prick Test
- Allergy Blood Test
For more complex cases, doctors may suggest additional diagnostic tests:
- Nasal Allergen Challenge (NAC)
- Basophil Activation Test (BAT)
- Olfactory Tests
- Quantification of Inflammatory Mediators
Treatment
Effective management of allergic rhinitis involves a combination of medications, immunotherapy, and lifestyle adjustments.
- Allergic Rhinitis Medication
- Antihistamines are often the first line of defence, blocking the effects of histamine released during allergic reactions.
- Nasal corticosteroids are considered the most effective medications for many people with hay fever.
- Decongestants provide short-term relief from nasal stuffiness and pressure
- For severe cases, doctors may recommend oral corticosteroids like prednisone for short-term use
- Immunotherapy
- Immunotherapy either through injections (allergy shots) or sublingual tablets.
When to See a Doctor
Consult a doctor if allergic rhinitis symptoms interfere with daily life, work performance, or sleep patterns. Persistent congestion, coughing, or watery eyes that disrupt sleep or make it challenging to function at work deserve medical attention. Additionally, a doctor can suggest alternative allergic rhinitis treatments if over-the-counter medications cause unwanted side effects like drowsiness.
Individuals with other health conditions such as heart disease, thyroid disease, diabetes, glaucoma, high blood pressure, enlarged prostate, liver disease, or kidney disease should always consult a doctor before self-treating allergies.
Prevention
Prevention is the most effective allergic rhinitis treatment at home. Preventing allergic rhinitis involves managing allergies before the body can respond adversely to substances.
- Pollen:
- If pollens trigger allergies, taking antihistamines preemptively can help.
- Staying indoors during peak pollen hours
- Showering immediately after being outside
- Keeping windows closed during allergy season
- Avoiding line-drying laundry outdoors
- Dust Mites:
- To reduce exposure to dust mites, create an inhospitable environment for their development:
- Wet mop hard floors instead of sweeping
- Use a vacuum with a HEPA filter for carpets
- Dust hard surfaces frequently
- Wash bedding weekly in hot water
- Use allergen-blocking pillows and cases
- Pet Dander:
- Limit exposure to animals that trigger allergies
- Clean all surfaces often
- Wash hands immediately after touching pets
- Keep pets off beds
- Wash clothes after visiting homes with pets
- Bathe dogs at least twice per week to minimise dander
Conclusion
Prevention is one of the most essential part in managing allergic rhinitis. By implementing methods to reduce exposure to allergens and creating allergy-friendly environments, individuals can minimise the frequency and severity of their symptoms. Regular consultations with doctors ensure that treatment plans remain effective and up-to-date. With proper management and a proactive approach, those affected by allergic rhinitis can lead comfortable and fulfilling lives, regardless of the season or their surroundings.
FAQ's
1. When do people usually get hay fever?
Hay fever can be seasonal, occupational, or even perennial (year-long). Generally, people experience hay fever during the following seasons:
- Spring (late April and May): Tree pollen is the primary culprit during this time.
- Summer (late May to mid-July): Grass and weed pollen are the primary triggers.
- Fall (late August to the first frost): Ragweed pollen is the most common cause.
2. How common is allergic rhinitis (hay fever)?
Allergic rhinitis is a widespread condition affecting millions of people worldwide. In the United States alone, it impacts an estimated 30% of people, making it one of the most common chronic conditions.
3. How many days does allergic rhinitis last?
The duration of allergic rhinitis symptoms can vary significantly and depends on the type of allergen, the individual's sensitivity, and environmental conditions. Seasonal allergies can last several weeks or even months as long as the triggering allergen remains in the environment. Perennial allergies can persist year-round due to constant exposure to indoor allergens like dust mites or pet dander.
4. What's the primary difference between hay fever and allergies?
While the terms "hay fever" and "allergies" are often used interchangeably, there are some distinctions to be aware of:
|
Condition |
Hay fever |
Allergies |
|
Definition |
A specific allergic reaction affects the nose and eyes (also known as allergic rhinitis) |
A broader term encompassing various allergic reactions |
|
Symptoms |
Runny nose, sneezing, congestion, itchy eyes, throat irritation (no fever) |
Vary depending on the type (respiratory issues, skin rashes, digestive problems, anaphylaxis) |
|
Triggers |
Airborne allergens (pollen, dust mites, mould spores, pet dander). |
A vast array of substances (foods, medications, insect stings, environmental factors) |
|
Duration |
Seasonal or perennial (depending on allergens). |
Seasonal, perennial, or sporadic (depending on exposure). |
|
Treatment |
Antihistamines, nasal corticosteroids, avoidance of triggers. |
Varies depending on type/severity (antihistamines to epinephrine for severe reactions) |
Dr Manoj Soni
General Medicine

Still Have a Question?



