-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals
Grade 1 Fatty Liver: Symptoms, Causes, Treatment and Diet Tips
Updated on 21 February 2024

Table of Content
- Grade 1 Fatty Liver
- Grade 1 Fatty Liver Symptoms
- What Causes and Increases Risks of Grade 1 Fatty Liver?
- Treatment Options
- When to See a Doctor
- Diet for 1st Grade Fatty Liver
- Diagnosis of Grade 1 Fatty Liver
- Prevention and Reversal Strategies of Grade 1 Fatty Liver
- Complications of Grade 1 Fatty Liver
- Is grade 1 fatty liver dangerous?
- Conclusion
- FAQs
One of the earliest and mildest stages of fatty liver disease is known as grade 1, or mild hepatic steatosis. While often displaying no overt clinical manifestations initially, grade 1 fatty liver marks the first step in liver metabolic dysfunction. Without timely intervention, it can silently progress to more serious inflammatory liver disease over the years.
This blog provides an informative overview of grade 1 fatty liver. We will discuss everything from its subtle signs and underlying reasons to practical lifestyle diet and tips to resolve it.
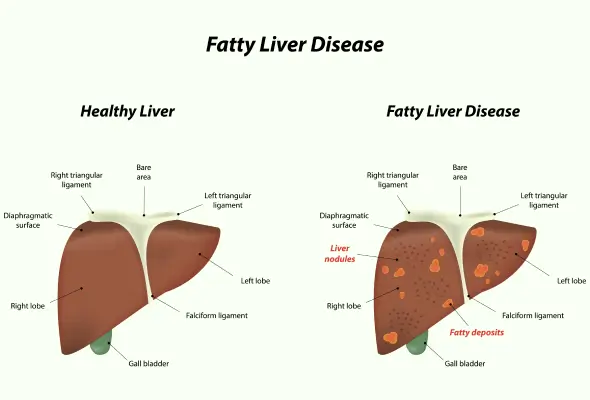
Grade 1 Fatty Liver
It is the early and the least severe stage of non-alcoholic fatty liver disease NAFLD. This is commonly known by the accumulation of fat in 5% to 10% of hepatocytes. Therefore, early diagnosis and treatment are key for eliminating progression to more advanced stages.
Grade 1 Fatty Liver Symptoms
Many people with grade 1 fatty liver do not show any clear symptoms. However, some subtle signs to watch out for include:
- Fatigue and weakness
- Upper abdominal discomfort
- Elevated liver enzymes
- High triglyceride levels
- Unexplained weight gain
- Impaired blood sugar control
What Causes and Increases Risks of Grade 1 Fatty Liver?
Some common causes of grade 1 fatty liver are:
- Obesity
- Insulin resistance and diabetes mellitus
- Dyslipidemia
- Unhealthy eating habits
- Losing weight too fast
- Certain medicines including corticosteroids, chemotherapy drugs, antiretroviral drugs
- Genetic predisposition
Additionally, those at greatest risk for having grade 1 fatty liver include those who:
- Have metabolic syndrome or its individual components such as obesity, hypertension, hyperglycemia, dyslipidemia.
- Have a sedentary lifestyle
- Eat processed carbohydrates, sugar, and high saturated fat foods.
Treatment Options
The treatment of grade 1 fatty liver centres around lifestyle improvement. Key strategies include:
- Weight Loss: Losing 3 to 5% of body weight through healthy eating and exercise goes a long way in reducing liver fat.
- Dietary Changes: Shifting to a Mediterranean style diet high in fruits, vegetables, whole grains, legumes, fish and healthy fats while limiting sugar, refined grains and unhealthy fats.
- Exercise: Getting 150-300 minutes of moderate intensity physical activity per week aids weight loss and metabolic health.
- Limit Alcohol: Avoiding heavy alcohol consumption allows the liver to recover.
- Treat Underlying Conditions: Seeking medical management of associated health issues like diabetes, high cholesterol and high blood pressure prevents progression of liver damage.
- In many cases, the above measures successfully resolve grade 1 fatty liver. However, if the disease advances despite lifestyle interventions, medications may be required.
When to See a Doctor
Consult a gastroenterologist or hepatologist promptly if you experience potential fatty liver symptoms or have risk factors like obesity and metabolic problems. Early detection allows to stop or reverse liver damage when it is still in its early stages.
Doctors can confirm the diagnosis using blood tests, imaging studies and sometimes liver biopsy. They may also initiate appropriate monitoring and treatment protocols based on disease severity.
Diet for 1st Grade Fatty Liver
A healthy diet and nutrition is a major part of the grade I fatty liver treatment. Follow these guidelines to improve your diet:
- Focus on plant foods: Firstly, prioritise fruits, vegetables, whole grains, nuts, seeds and legumes that are rich in good fats, fibre, vitamin minerals and antioxidants which help repair the liver.
- Opt for lean protein sources: Add fatty fish, poultry without skin, soy products, legumes, low fat dairy and eggs to support your liver health.
- Say no to deep fried food: Avoid deep-fried foods or ultra-processed foods
- Lower sugar consumption: Control insulin resistance by minimising sugar-sweetened beverages, canned fruits in sweet syrup and refined carbohydrates, (such as the sugary drinks)
- Increase omega-3 intake: Eat more omega-3 fatty acids from fish; chia seeds, walnuts as well flaxseeds because they have anti-inflammatory effects on the liver.
- Keep hydrated: Drink enough fluids, especially water. Include lemon for antioxidants protection. Minimise alcohol use.
Diagnosis of Grade 1 Fatty Liver
Diagnosing grade 1 fatty liver often occurs without noticeable symptoms and may be discovered during routine medical examinations or while conducting tests for other health reasons. If liver abnormalities are detected on ultrasound or if liver enzyme tests show anomalies, additional diagnostic tests are usually ordered to confirm the presence and assess the severity of fatty liver disease.
To determine and evaluate fatty liver disease, doctors use various diagnostic tests:
- Blood Tests: These include liver enzyme tests (liver function tests), complete blood count (CBC), tests for chronic viral hepatitis, screening for celiac disease, fasting blood sugar levels, hemoglobin A1C test, and lipid profile.
- Imaging Procedures: These could include magnetic resonance elastography and transient elastography to measure liver stiffness, as well as abdominal ultrasonography, CT scan, or MRI
- Liver Biopsy: In cases where other tests do not provide conclusive results, a liver biopsy may be recommended. This involves obtaining a small tissue sample from the liver using a needle, which is then examined under a microscope for signs of inflammation and scarring.
Prevention and Reversal Strategies of Grade 1 Fatty Liver
Currently, there are no established medical or surgical treatments specifically for fatty liver. However, there are preventive and reversal strategies that can help mitigate its effects.
If you have fatty liver, here are recommended actions:
- Aim to lose weight gradually, targeting half to one kilogram (one to two pounds) per week.
- Lower triglyceride levels through changes in diet, medication, or a combination of both.
- Completely abstain from alcohol consumption.
- Manage diabetes effectively if diagnosed.
- Adopt a balanced diet that's low in salt and sugar, emphasizing fruits, vegetables, and whole grains.
- Increase physical activity levels.
- Schedule regular appointments with a liver specialist.
- Before using any dietary supplements or herbal remedies, consult with your healthcare provider.
So, overall the most effective approach to preventing fatty liver disease involves maintaining a healthy weight, engaging in regular physical activity, limiting alcohol intake, and adhering to prescribed medical treatments.
Complications of Grade 1 Fatty Liver
If left untreated, grade 1 fatty liver can lead to serious complications:
- Chronic liver disease can progress to liver cirrhosis, where inflammation causes the formation of scar tissue (fibrosis) in the liver, impairing its function.
- Accumulation of fluid in the abdomen, known as ascites, may occur.
- Swelling of veins in the esophagus (esophageal varices) can develop, potentially leading to ruptures and bleeding.
- Hepatic encephalopathy, characterized by confusion, drowsiness, and slurred speech, may arise.
- There is an increased risk of liver cancer.
- Ultimately, untreated fatty liver might result in end-stage liver failure, which is caused by the liver's failure.
Is grade 1 fatty liver dangerous?
Grade 1 fatty liver, or mild hepatic steatosis, is generally not considered dangerous on its own. It indicates a mild accumulation of fat in the liver without significant damage. However, if not managed through lifestyle changes, it can progress to more severe liver conditions over time. Regular monitoring and healthy habits are crucial for preventing complications.
Conclusion
To sum up, grade 1 fatty liver indicates the earliest stage of NAFLD characterised by mild fat buildup in the liver. Common risk factors include obesity, insulin resistance, high blood fats and an unhealthy diet. Symptoms may be mild or absent initially. However, early detection and taking prompt action provide the best chance of reversing damage. With timely lifestyle interventions, individuals can halt and even reverse grade 1 fatty liver to restore normal liver health and function.
FAQs
1. Is grade 1 fatty liver dangerous?
No, grade 1 fatty liver is not dangerous on its own. It represents the earliest and mildest stage of NAFLD with minimal fat affecting less than 10% of liver cells. At this stage, there is no liver inflammation or scarring. However, without lifestyle intervention, it can silently progress to more serious inflammatory conditions like NASH, cirrhosis, and liver failure over years to decades.
2. Is grade 1 fatty liver normal?
No, any degree of liver fat accumulation is considered abnormal. Even grade 1 fatty liver indicates dysfunctional fat metabolism and insulin resistance and warrants attention.
3. How can I reduce my fatty liver grade 1?
Losing 3-5% of body weight through regular exercise and a healthy diet can effectively resolve grade 1 fatty liver in many cases. Limiting alcohol, reducing sugar/refined carbs, increasing fibre, drinking more water and managing conditions like diabetes and high cholesterol also support liver health.
4. What not to eat with a fatty liver?
Foods to avoid with a fatty liver include fast food, fried items, full-fat dairy, processed meats, sugary beverages, refined grains, and alcohol which drive liver fat accumulation. Focus on anti-inflammatory whole foods like vegetables, fruits, legumes, nuts, and fatty fish for liver protection.
5. Can alcohol consumption contribute to grade 1 fatty liver disease?
Yes, excessive alcohol consumption can contribute to the development of fatty liver disease, including grade 1. It can lead to fat accumulation in the liver cells, even without significant inflammation or damage.
6. What is the difference between grade 1 and grade 2 fatty liver disease?
Grade 1 fatty liver (mild hepatic steatosis) involves minimal fat accumulation in the liver cells with no inflammation or scarring. Grade 2 fatty liver (moderate hepatic steatosis) indicates a higher degree of fat accumulation, potentially with mild inflammation.
7. Is grade 1 fatty liver disease reversible?
Yes, grade 1 fatty liver disease is generally reversible with lifestyle changes such as weight loss, healthy diet, regular exercise, and abstaining from alcohol. These measures can reduce fat in the liver and improve liver health.
8. What does grade 1 fatty liver mean?
Grade 1 fatty liver means there is mild fat accumulation in liver cells without significant inflammation or liver damage. It is often detected incidentally during medical checkups or imaging tests.
9. Is grade 1 fatty liver and diabetes related?
Yes, there is a relationship between grade 1 fatty liver and diabetes. Insulin resistance, which is common in type 2 diabetes, can contribute to fat accumulation in the liver cells, leading to fatty liver disease.
10. What are the major symptoms of grade 1 fatty liver?
Grade 1 fatty liver typically does not cause symptoms in most people. However, some may experience fatigue, discomfort in the upper right abdomen, or mild enlargement of the liver.
11. Does drinking water flush the liver?
Drinking water is important for overall health, including liver function, but it does not directly flush toxins from the liver. Staying hydrated supports liver function by aiding in the removal of waste products and promoting overall health

ENQUIRY FORM
SELECT CATEGORIES
-
Neurosciences (16)
-
Neurology (37)
-
Neurosurgery (14)
-
Orthopaedics (48)
-
Oncology (33)
-
Obstetrics and gynecology (52)
-
Pulmonology (23)
-
Urology (20)
-
Nephrology (13)
-
Psychiatry (7)
-
Dietetics and Nutrition (111)
-
General Medicine (63)
-
Cardiac Sciences (32)
-
Vascular & Endovascular Surgery and Interventional Radiology (15)
-
Gastroenterology (46)
-
Endocrinology (23)
-
Plastic Surgery (10)
-
Critical Care Medicine (5)
-
COVID-19 (16)
-
Dermatology (16)
-
Emergency Care (1)
-
Ophthalmology (4)
-
Pediatrics (14)
-
Laparoscopic and Bariatric Surgery (8)
-
ENT (15)
-
Kidney Transplant (1)
-
Liver Transplantation and Hepatobiliary Surgery (5)
-
General Surgery (3)
-
Internal Medicine (5)
-
Medicine Information
Stomach Ulcer: Symptoms, Causes, Treatment and Home Remedies
Diet After Gallbladder Removal: What to Eat and What to Avoid
YOU MAY ALSO LIKE
RECENT BLOGS
-

Preterm Birth (Premature Birth): Symptoms, Causes, Treatment and Prevention
13 May 2025
Read More
-
Rotablation Angioplasty: Benefits, Treatments, And Recovery Time
9 May 2025
Read More
-

What Is The Difference Between IUI and IVF?
9 May 2025
Read More
-

Venous Malformations: Causes, Symptoms, and Treatment
30 April 2025
Read More
-
Varicose Vein Foam Sclerotherapy: Treatment, Benefits, and Procedure
30 April 2025
Read More
-
Radiofrequency (RF) Ablation Treatment for Varicose Veins: Know More
30 April 2025
Read More
-

Varicose Vein Sclerotherapy: Treatment, Benefits, and Procedure
30 April 2025
Read More
-
Varicose Vein Endovenous Laser Ablation: Procedure, Benefits, Risks
30 April 2025
Read More
Have a Question?
If you cannot find answers to your queries, please fill out the enquiry form or call the number below. We will contact you shortly.